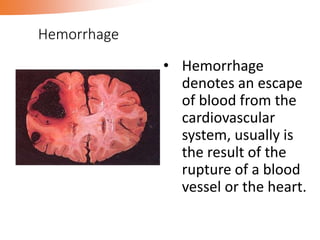
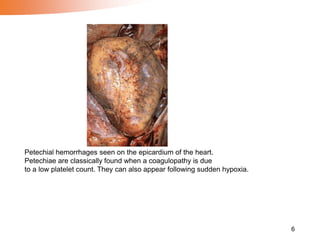
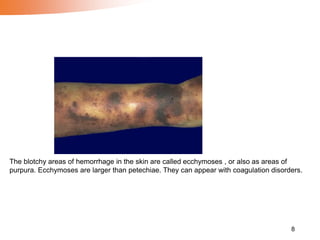
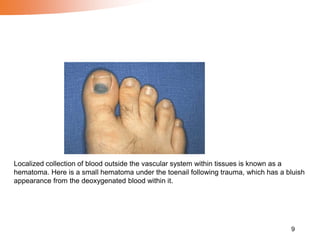
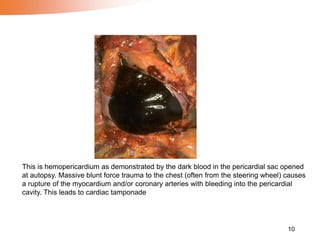
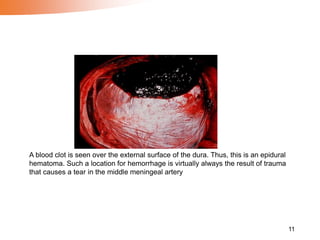
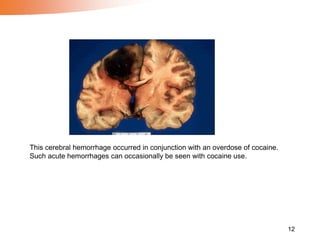
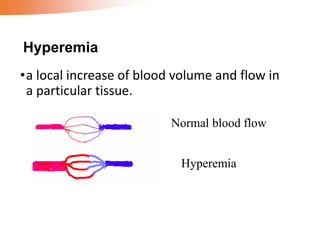
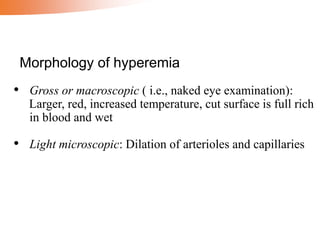
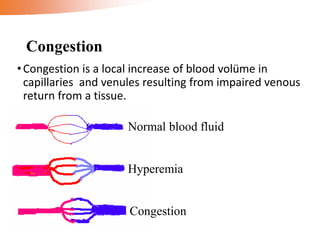
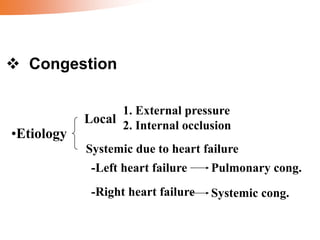
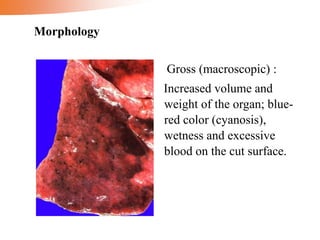
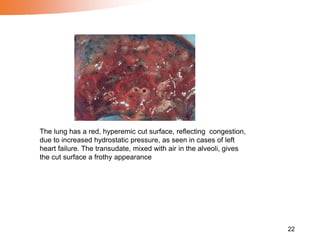
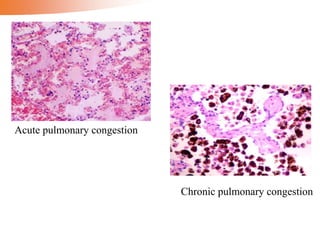
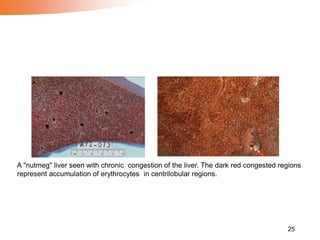
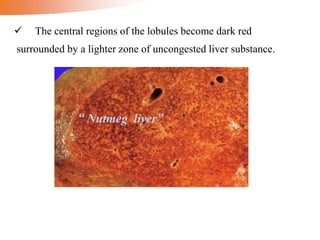
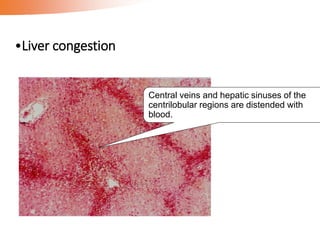
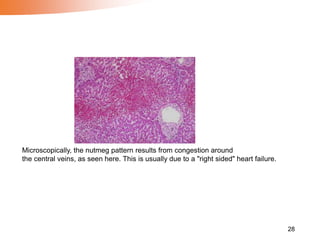
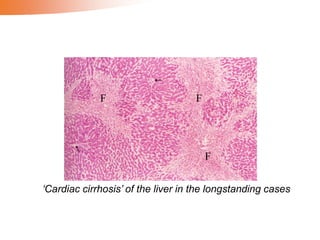
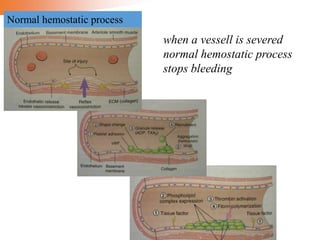
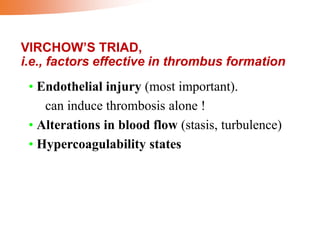
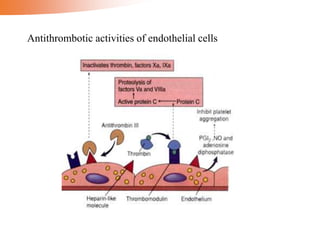
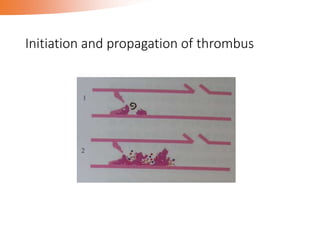
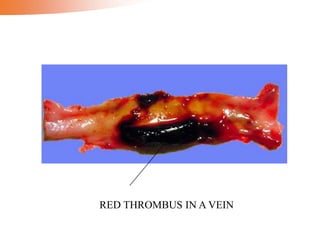
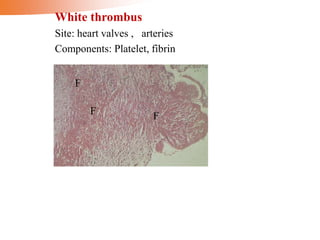
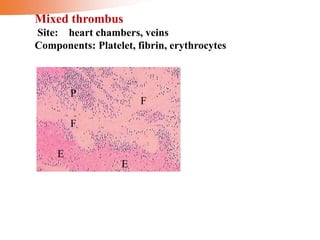
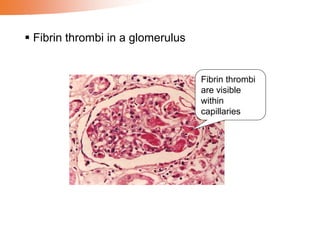
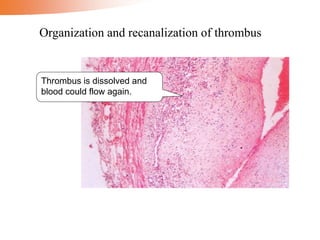
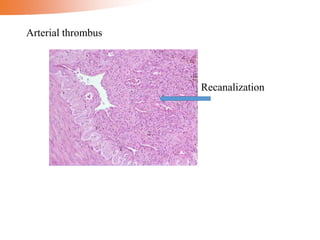
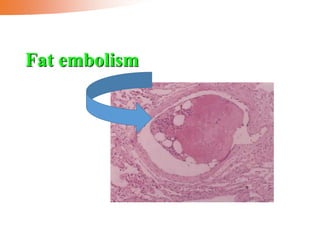
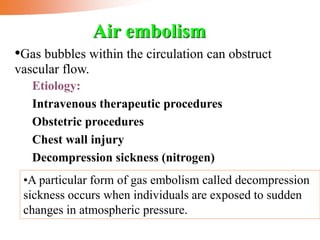
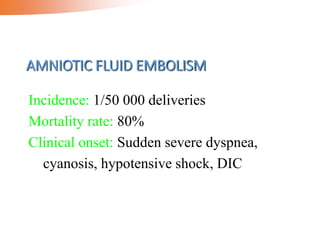
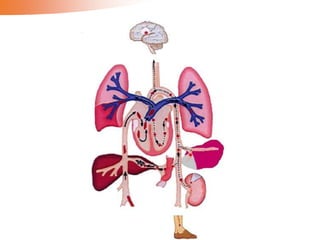
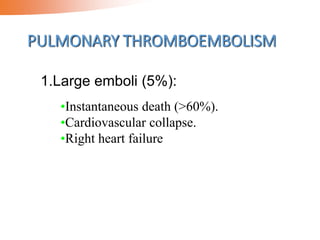
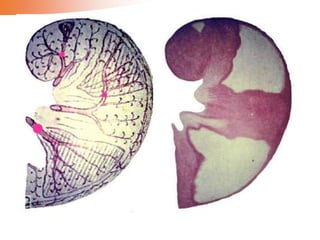
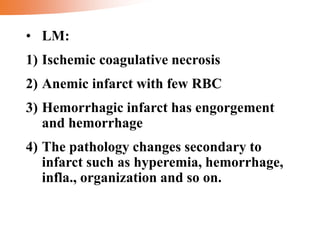
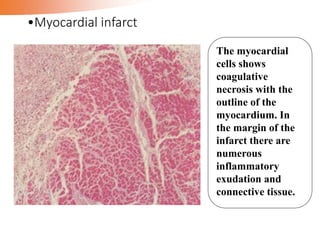
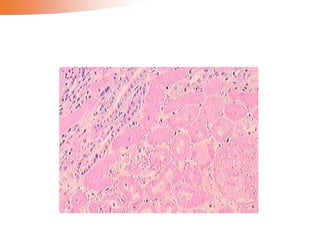
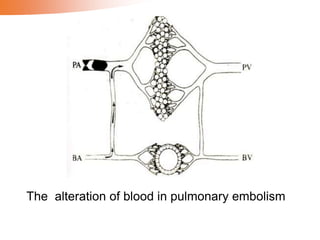
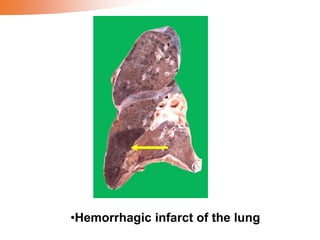
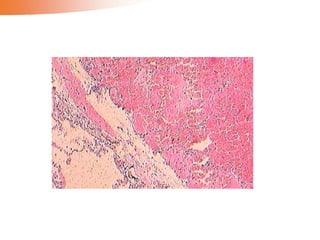
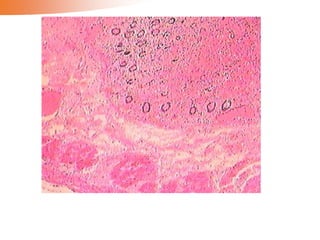
The document covers hemodynamic disorders, focusing on the pathological mechanisms related to bleeding, hyperemia, and thrombosis. It discusses various types of hemorrhage, their causes, and the physiological and pathological implications of increased blood volume and flow, including conditions related to thrombus formation and embolism. Additionally, it details infarction, its processes, morphology, and outcomes within different tissues and organs.