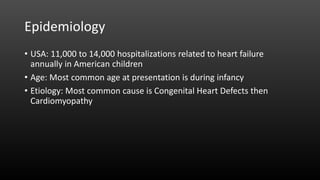
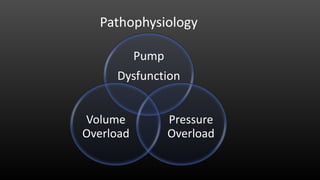
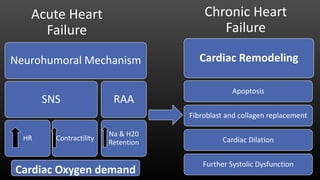
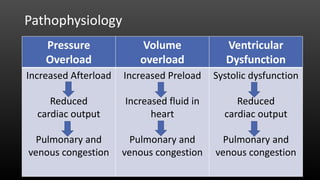
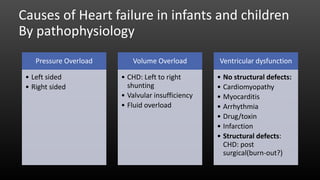
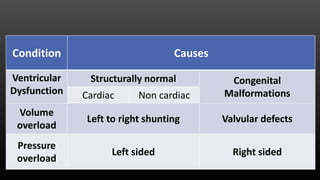
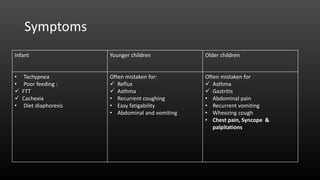
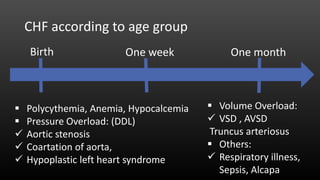
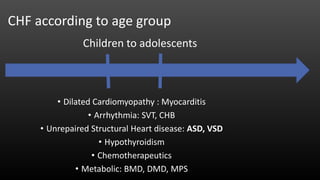
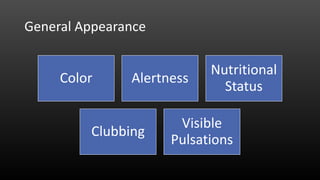
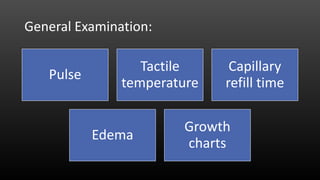
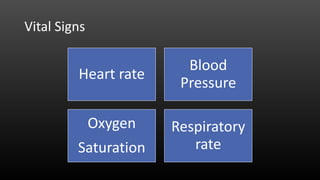
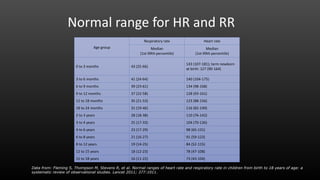
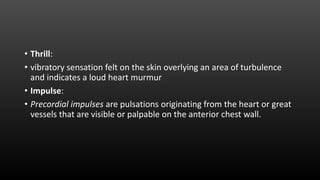
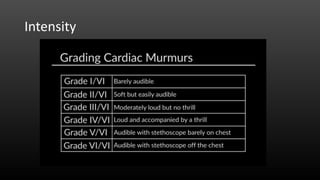
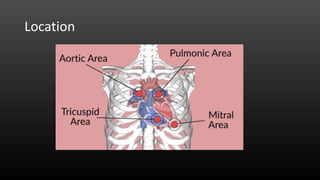
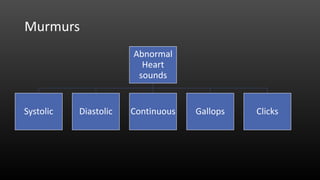
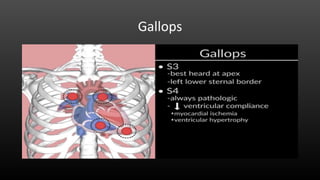
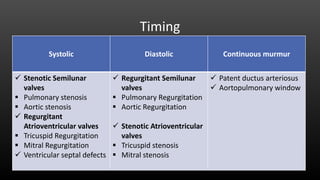
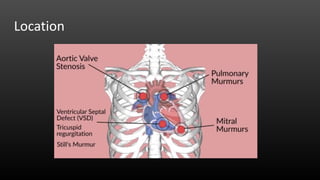
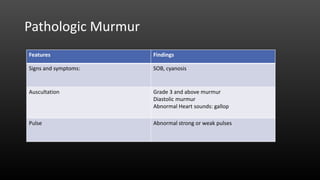
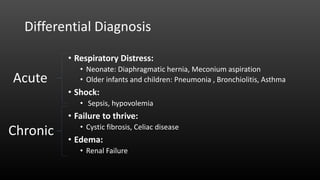
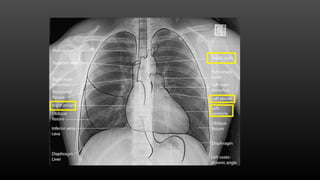
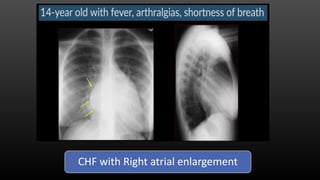
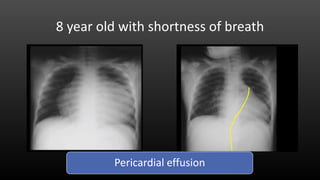
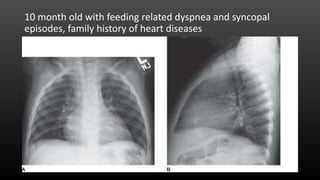
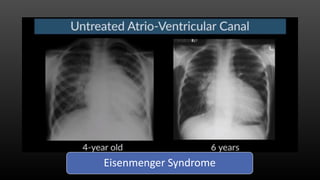
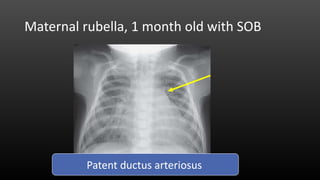
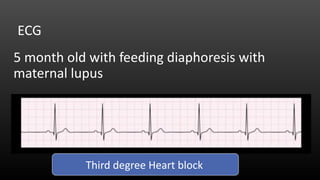
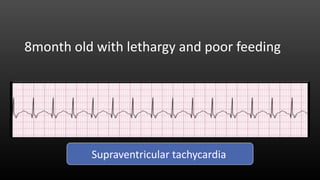
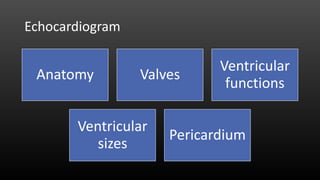
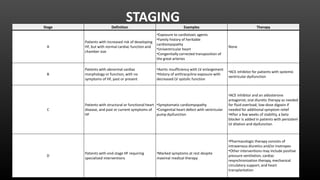
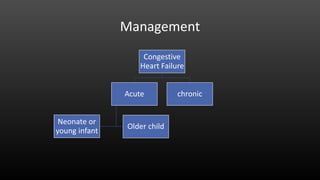
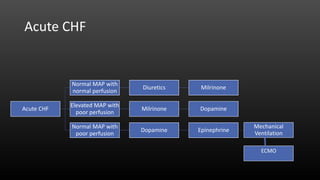
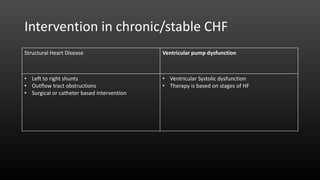
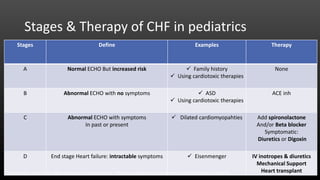
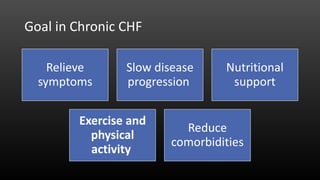
This document discusses congestive cardiac failure in children. It defines congestive cardiac failure as a state of systemic and pulmonary congestion resulting from impaired ability of the ventricle to fill or eject blood. The most common causes in children are congenital heart defects and cardiomyopathy. Symptoms vary by age but can include poor feeding, tachypnea, coughing, and fatigue. Diagnosis involves history, physical exam assessing vital signs, heart sounds and edema, as well as tests like echocardiogram, ECG and chest x-ray. Management depends on whether the failure is acute or chronic, and involves diuretics, inotropes, oxygen, surgery or catheter interventions, and long-term therapy based