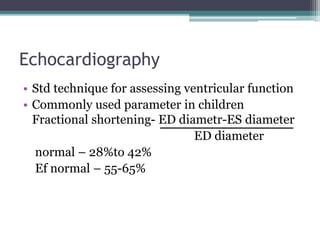
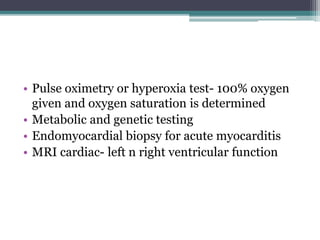
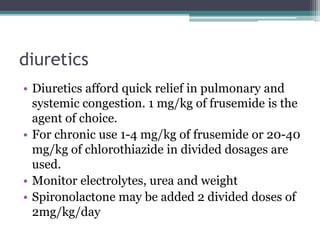
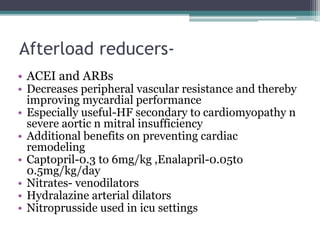
The document discusses heart failure in pediatric patients, detailing diagnostic methods such as chest radiography, echocardiography, and laboratory investigations to assess cardiac function. It outlines treatment strategies, including medical management with diuretics, afterload reducers, and inotropes, along with general care measures and dietary recommendations. Additionally, it emphasizes the importance of addressing underlying causes and considerations for acute cases requiring ICU admission.