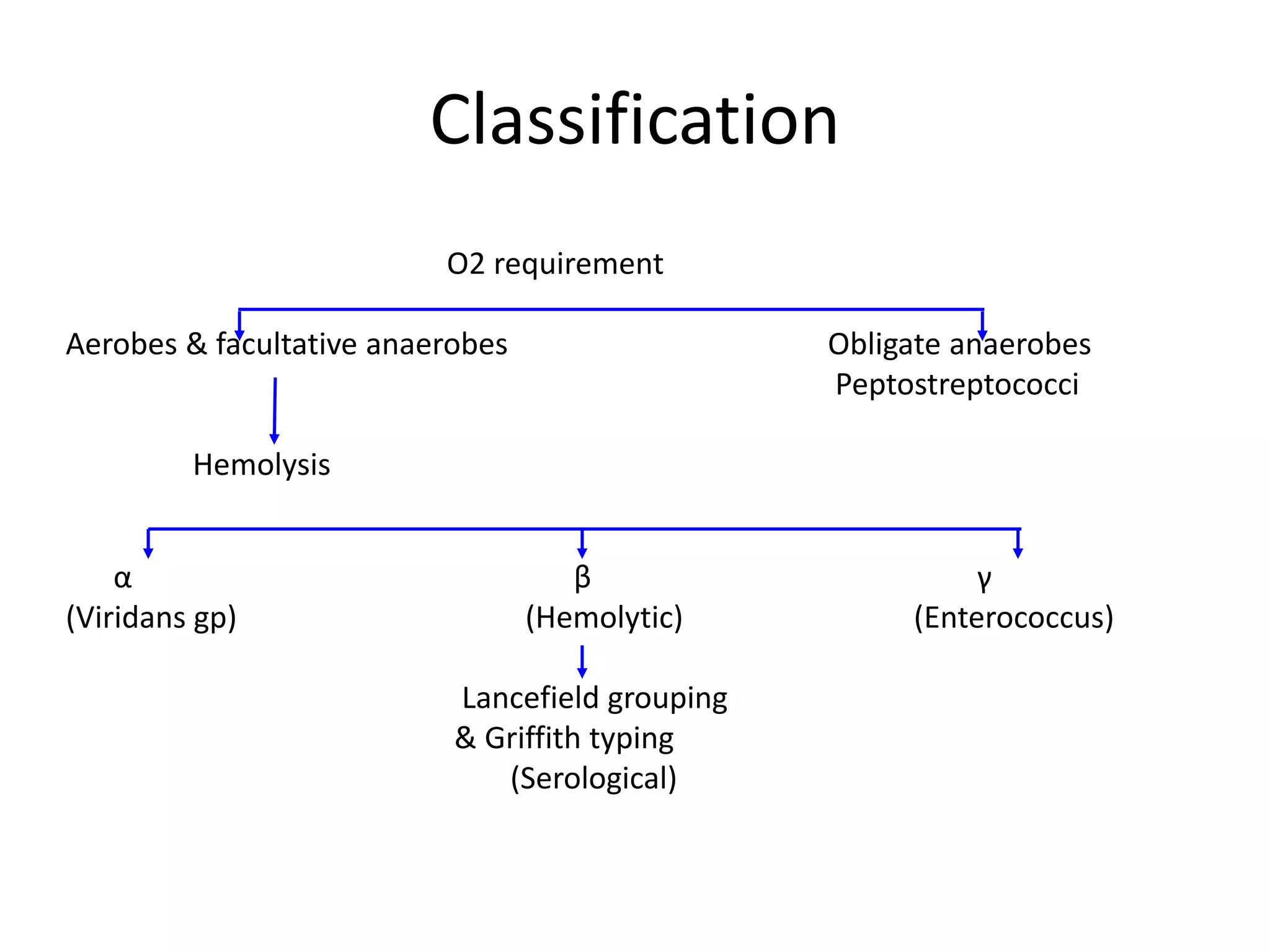
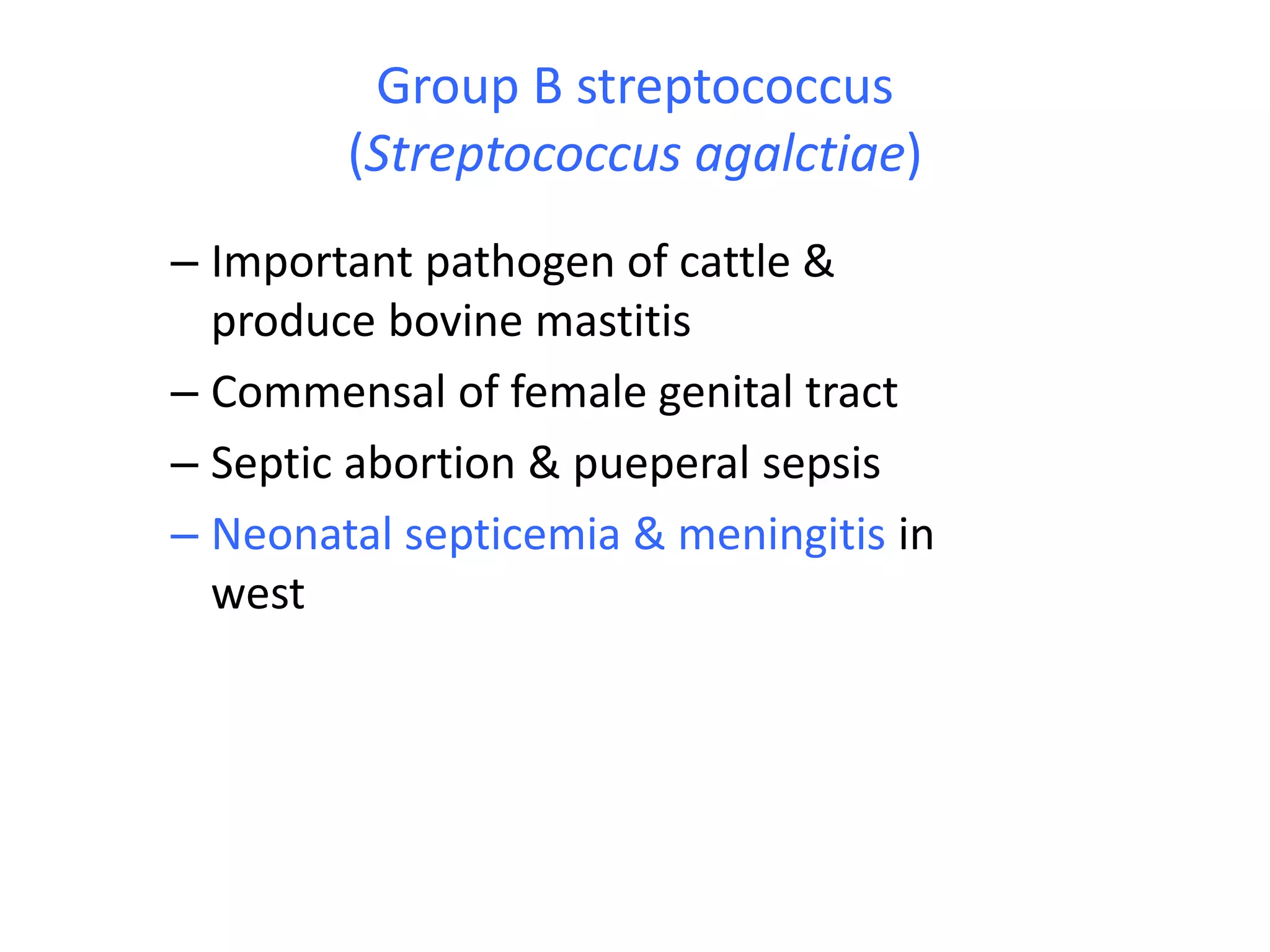
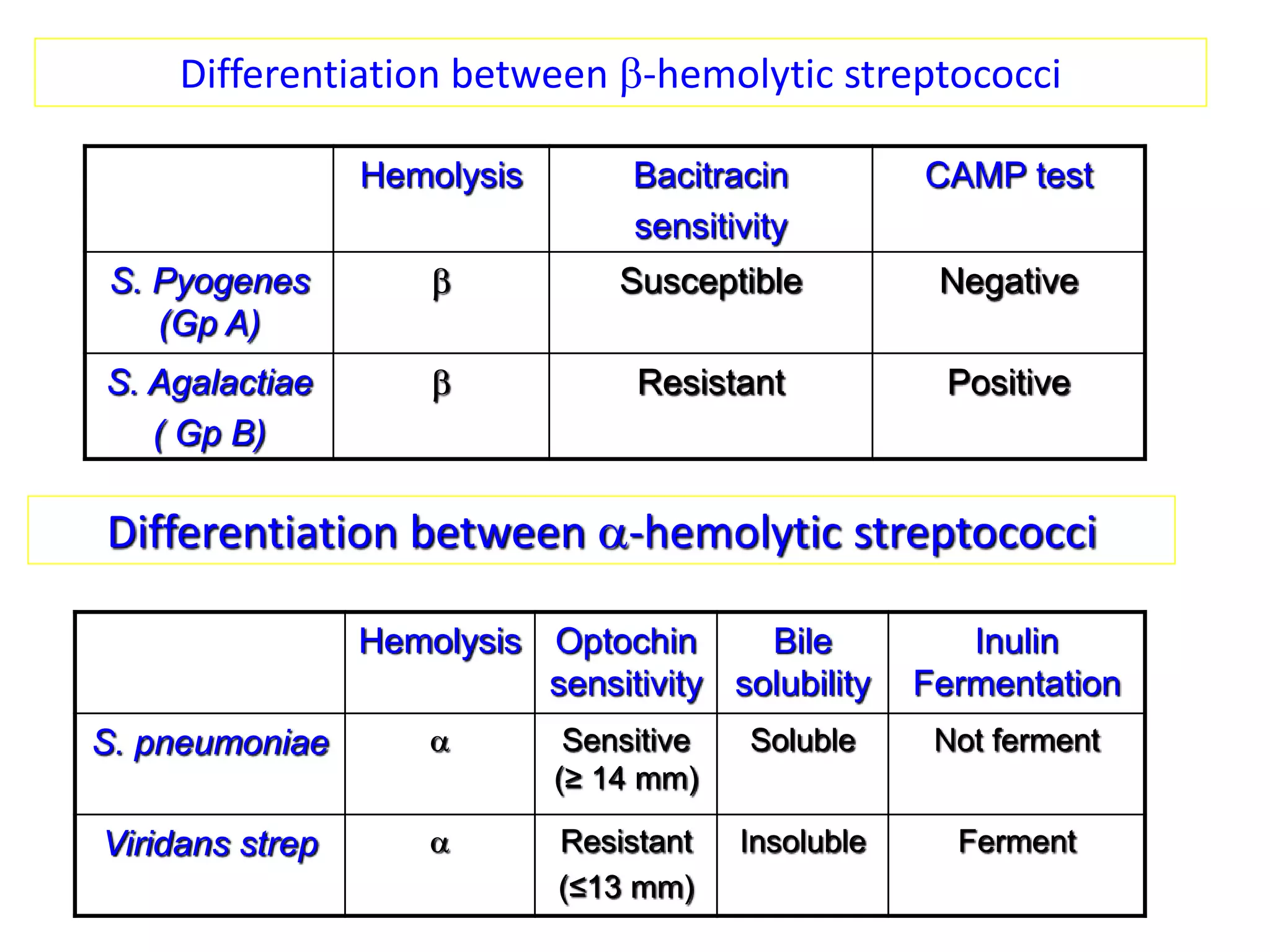
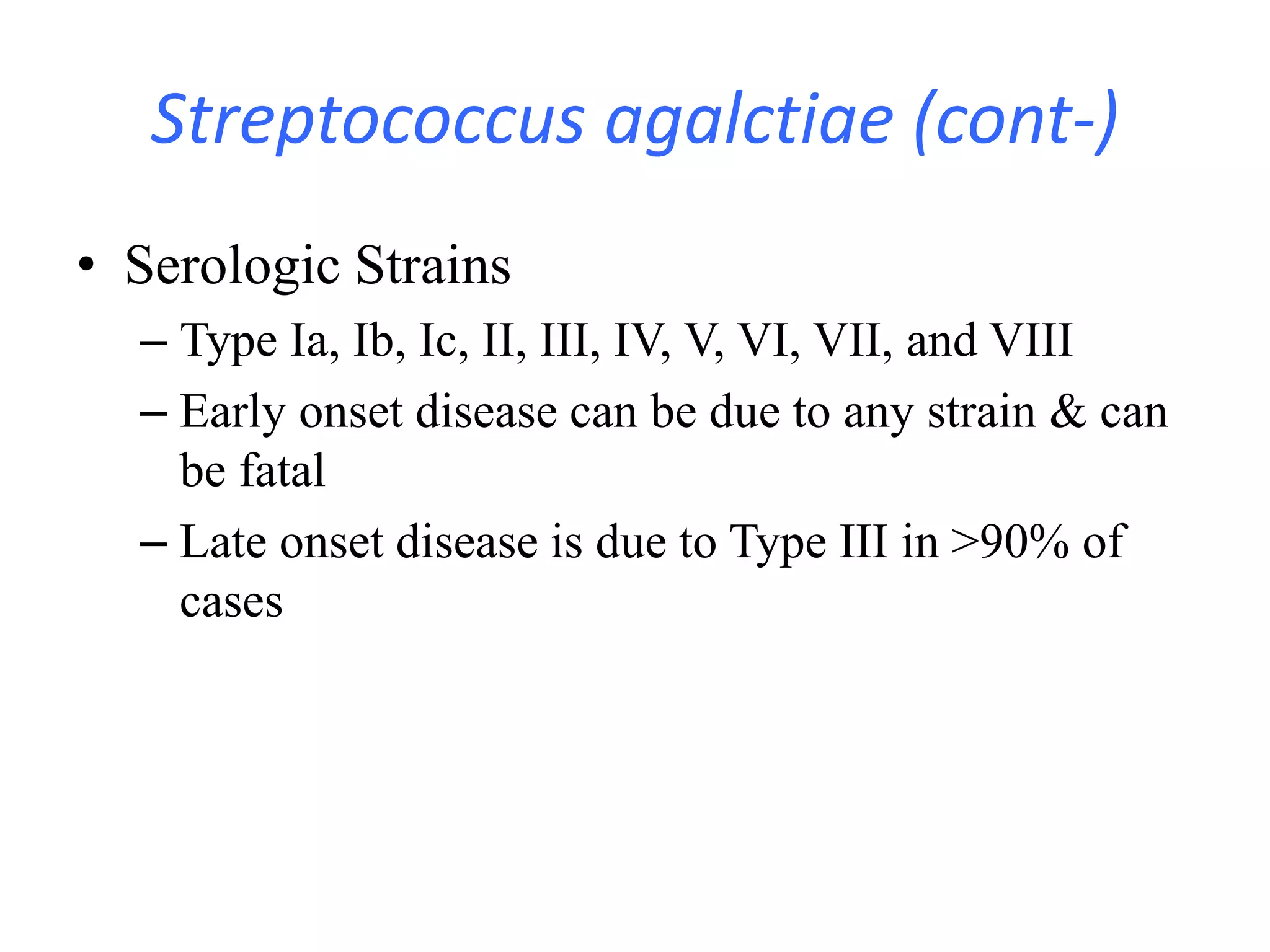
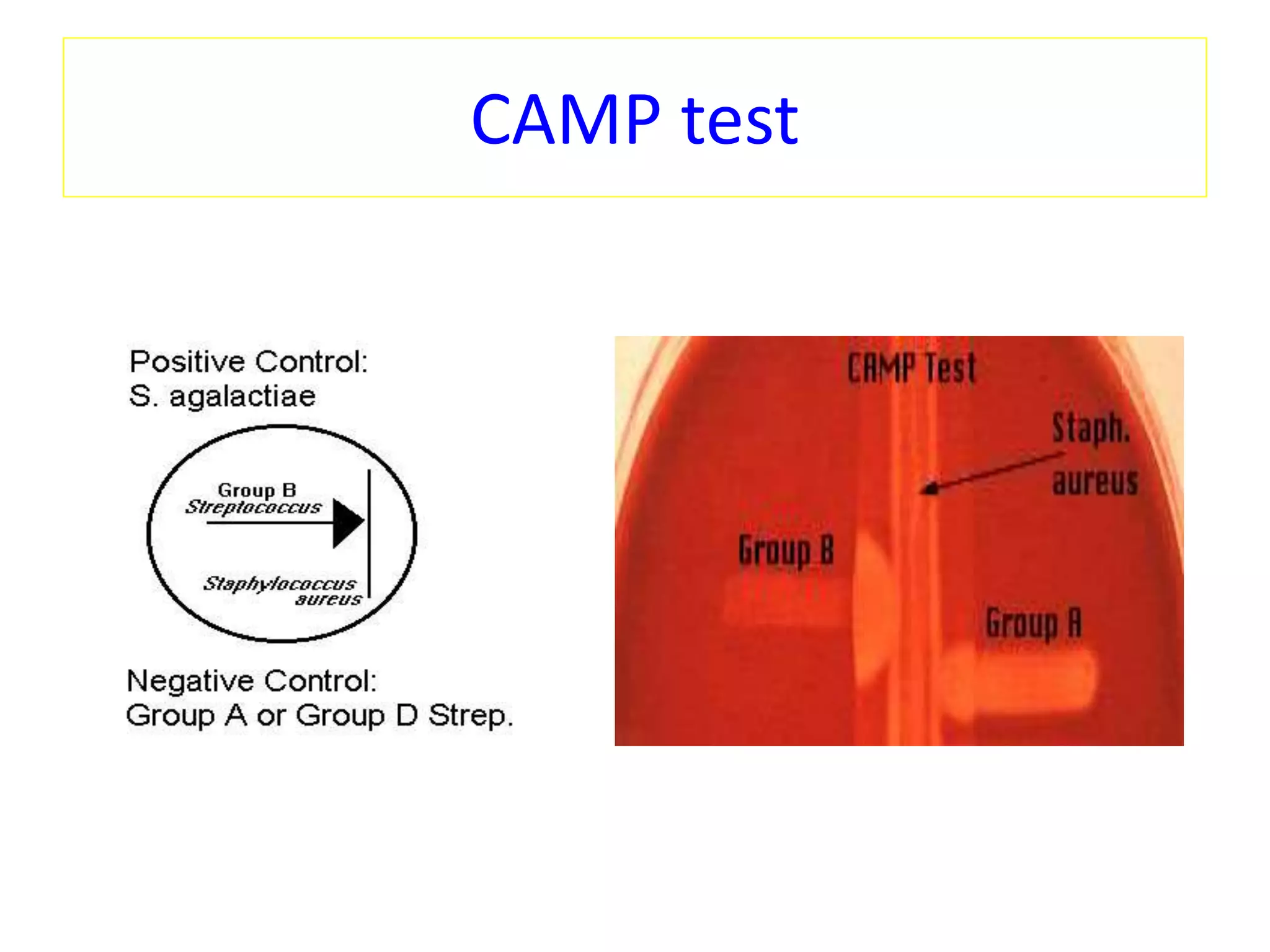
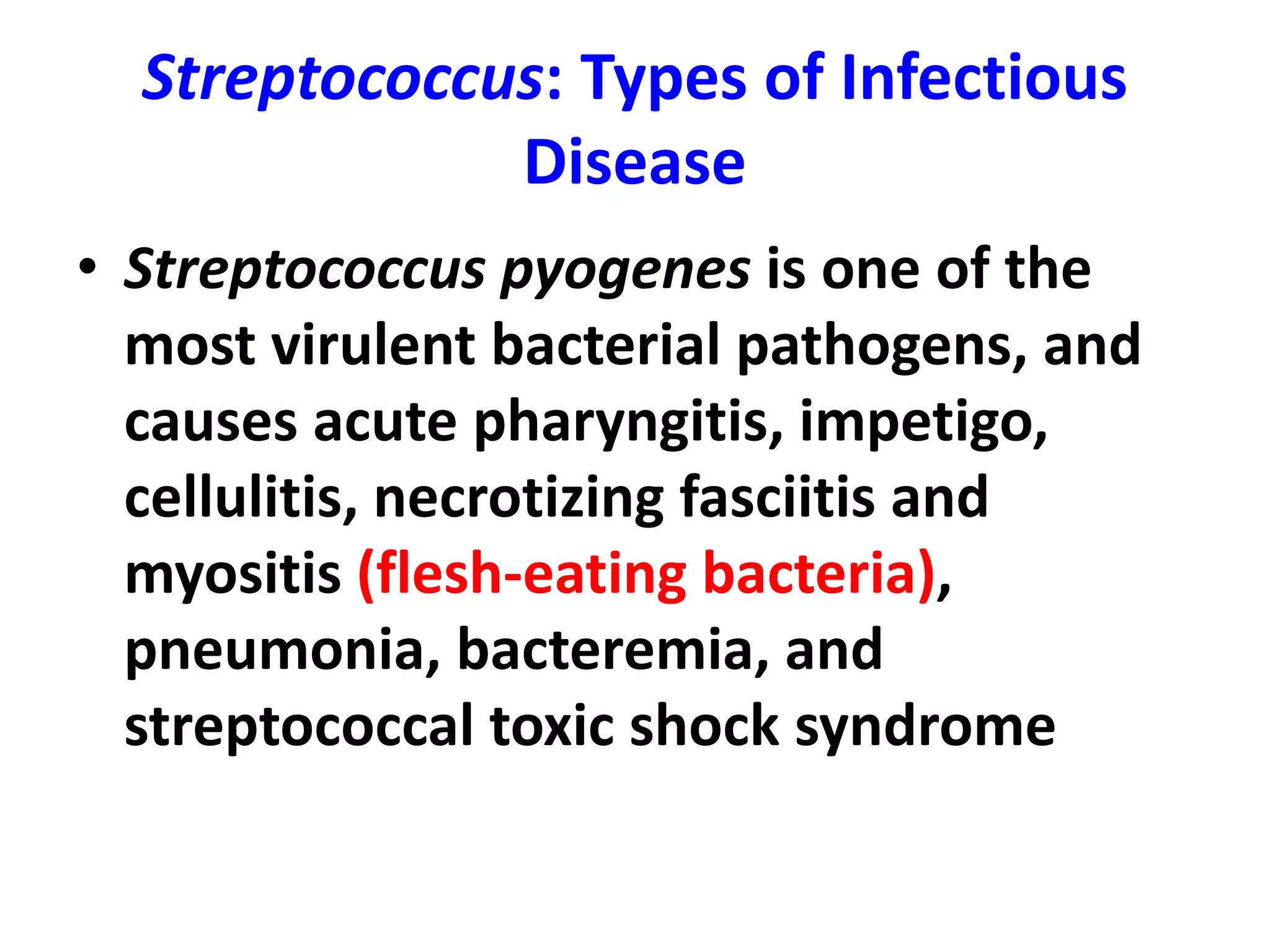
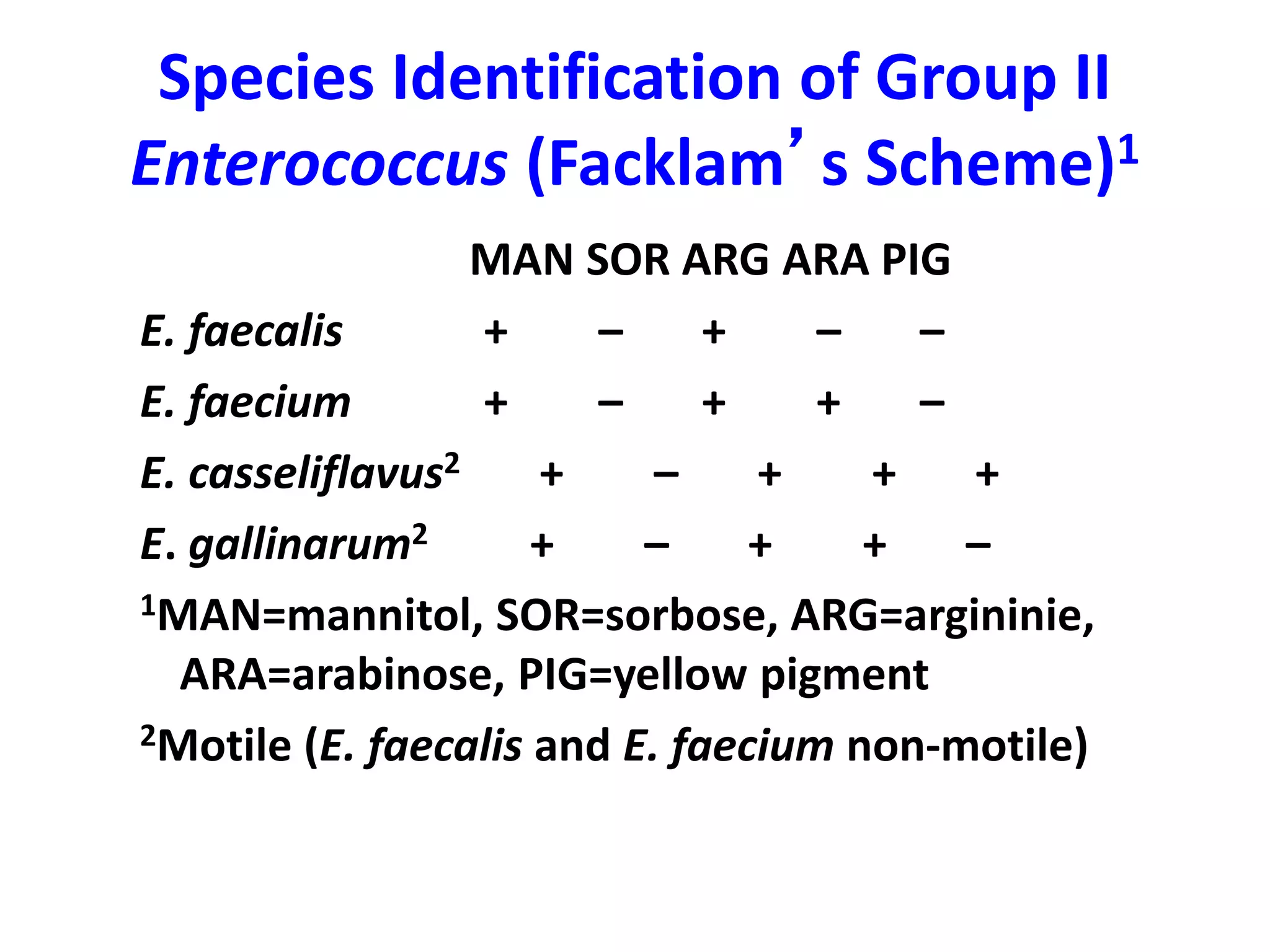
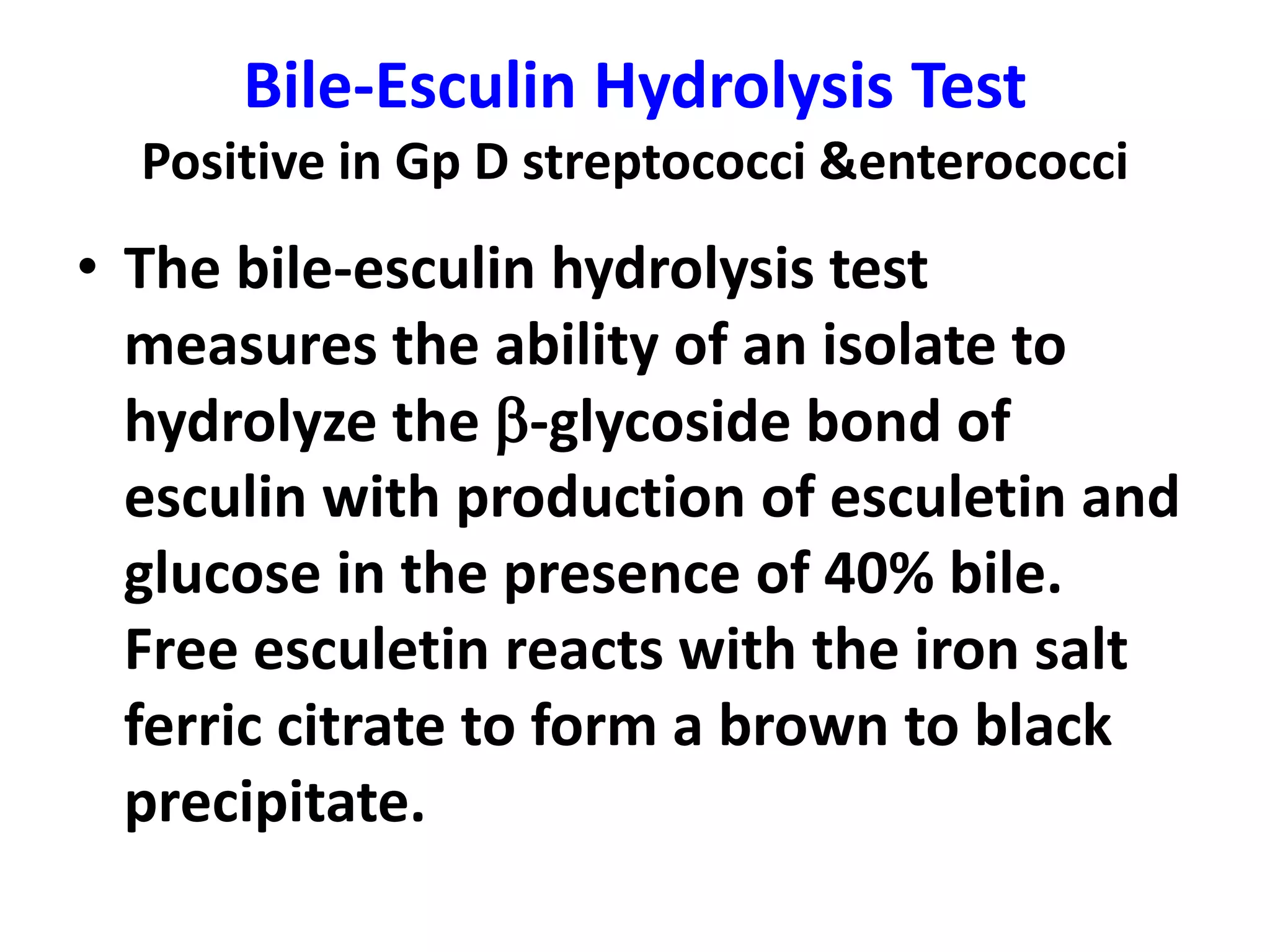
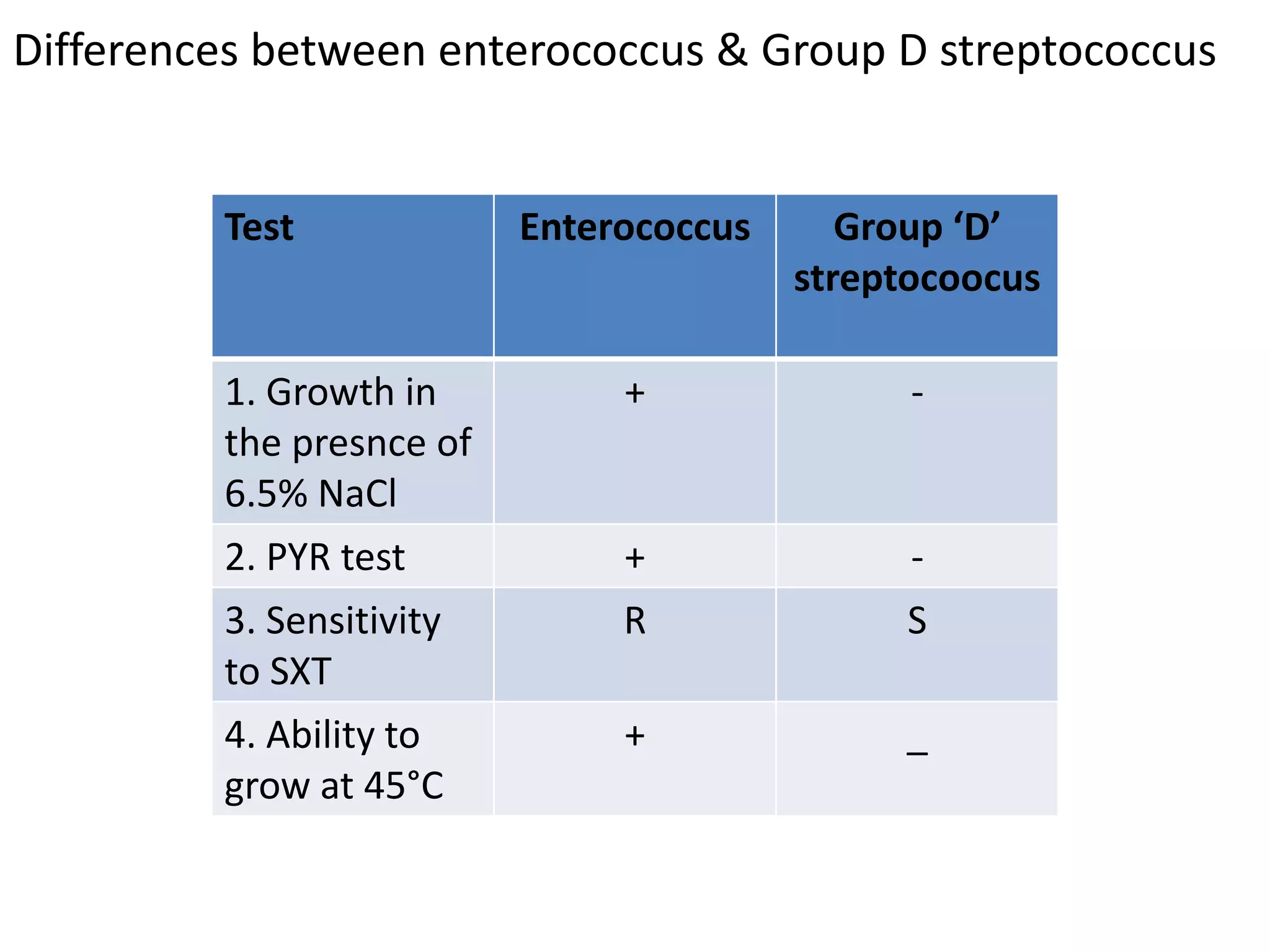
This document summarizes key information about Group B and Group D streptococci. It discusses their classification, pathogenicity, laboratory identification tests like hemolytic patterns on blood agar, CAMP test, bacitracin sensitivity test, and characteristics that differentiate streptococcal species. Information provided includes diseases caused by Streptococcus agalactiae (Group B strep), Enterococcus faecalis, and the differences between enterococci and non-enterococcal Group D streptococci.