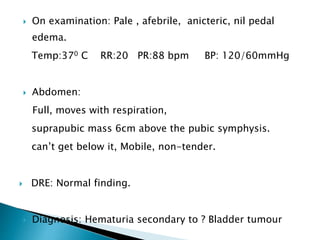
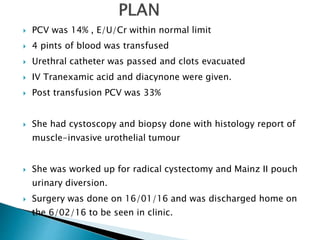
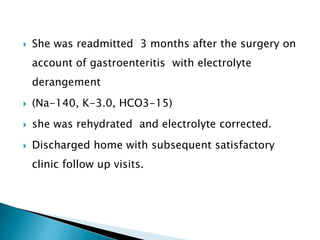
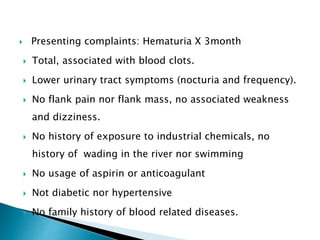
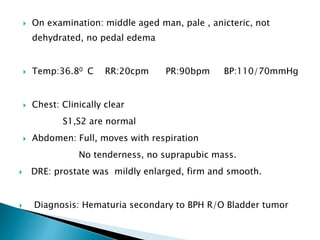
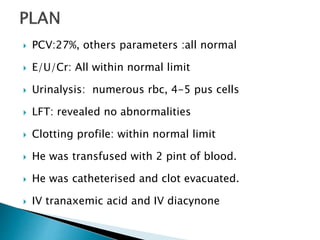
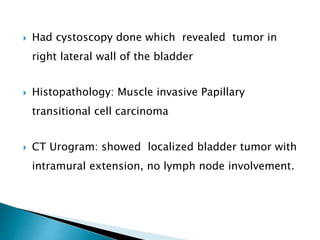
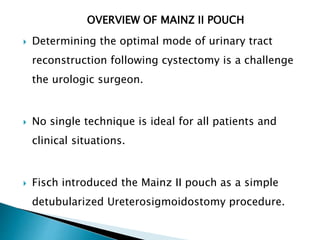
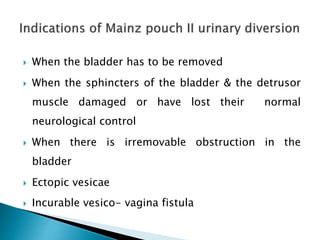
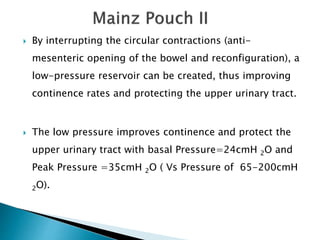
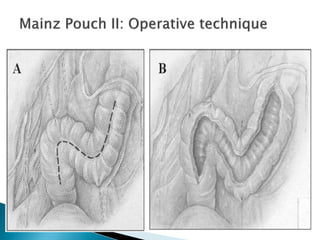
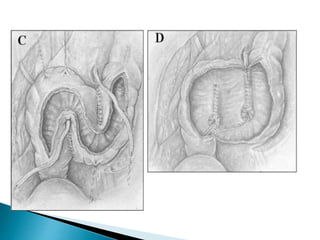
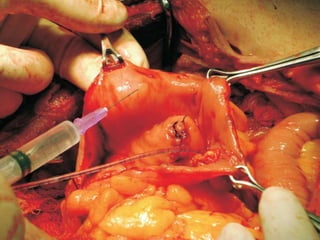
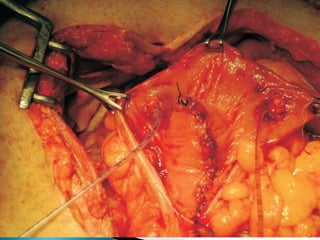
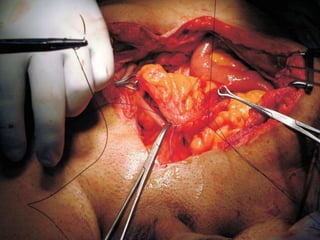
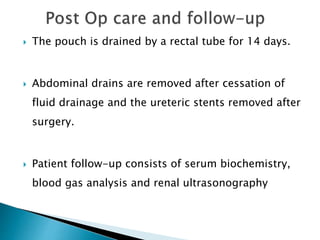
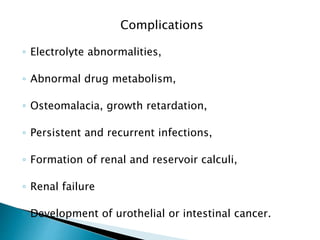
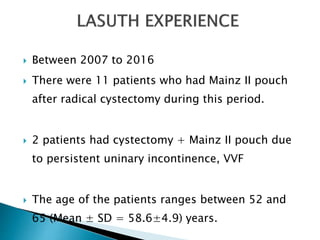
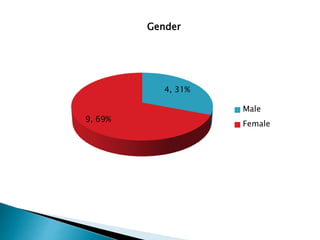
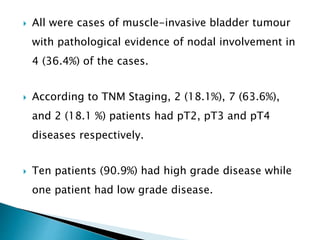
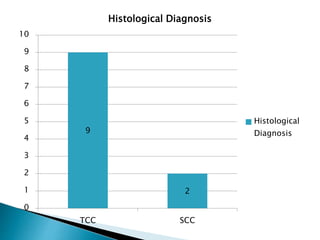
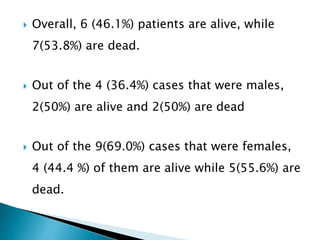
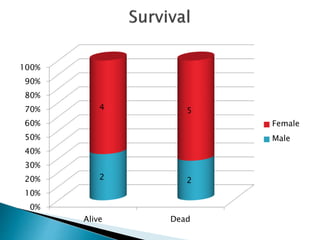
The document details two case presentations of patients with hematuria leading to diagnoses of bladder tumors, both requiring surgeries involving radical cystectomy and Mainz II pouch urinary diversion. It illustrates the historical development and complications associated with urinary diversion techniques, particularly the Mainz II pouch, which aims to provide a continent and low-pressure reservoir for urinary management. The outcomes of the surgeries are discussed, highlighting post-operative complications and the importance of monitoring patient survival and quality of life.