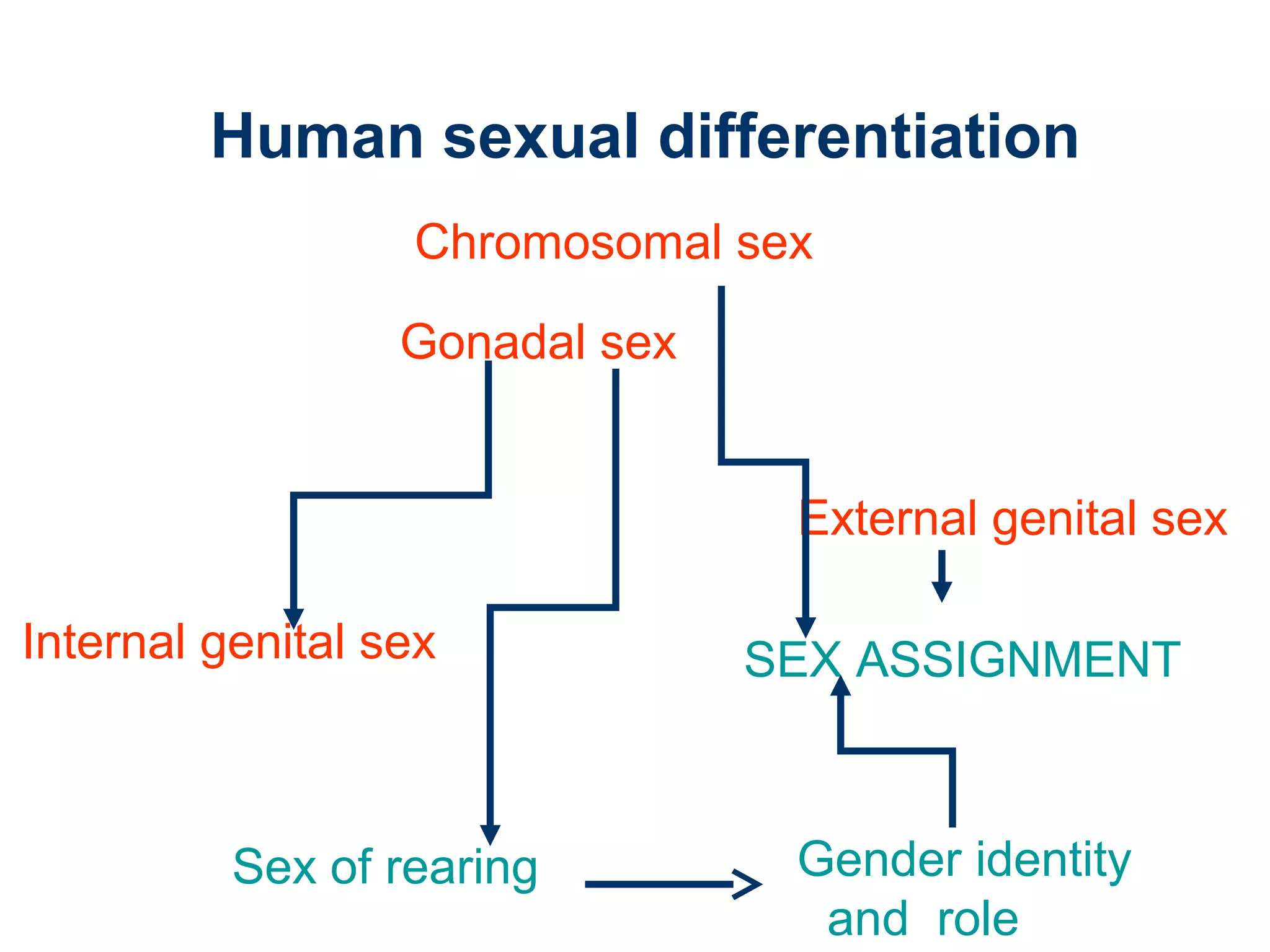
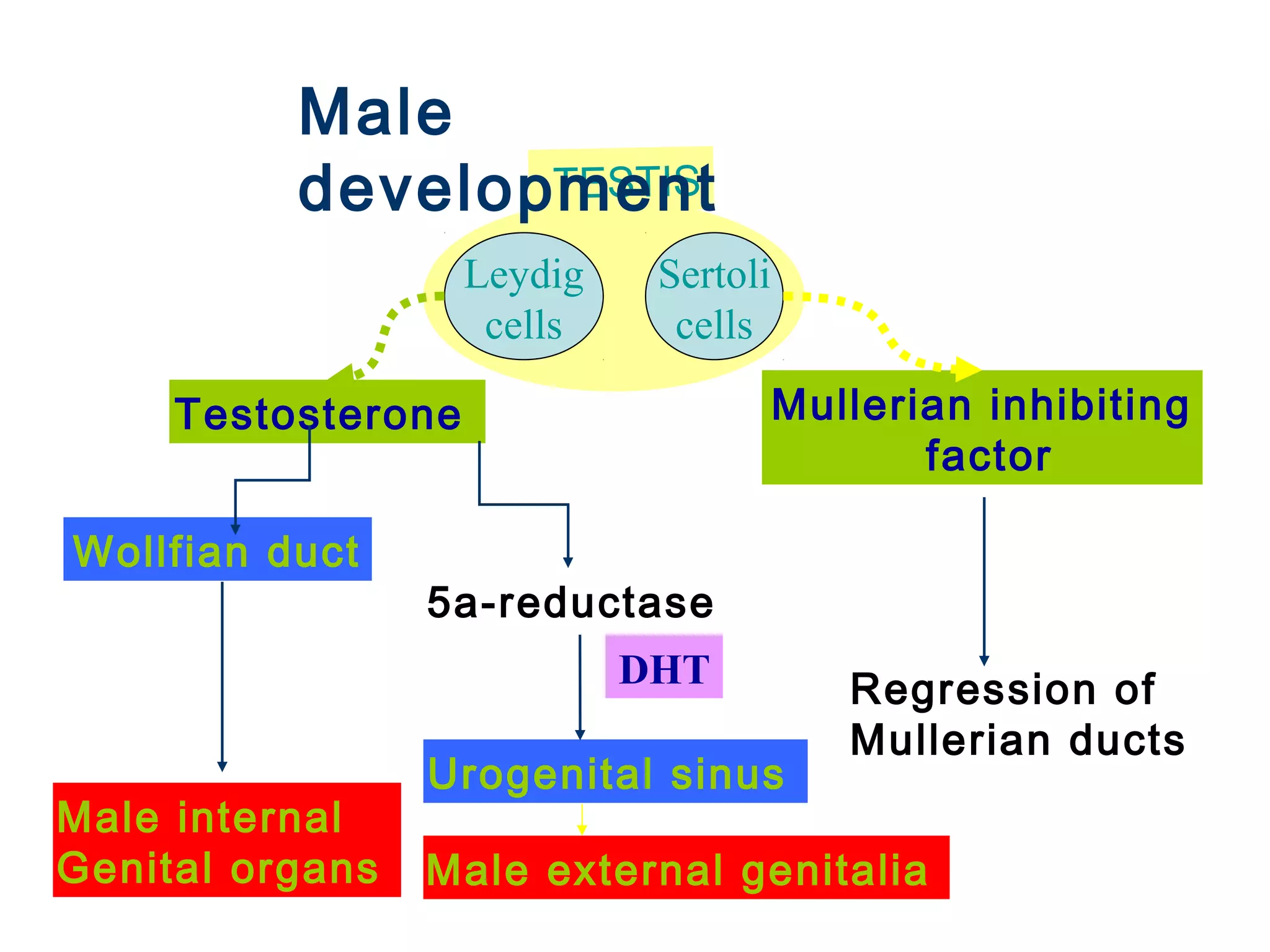
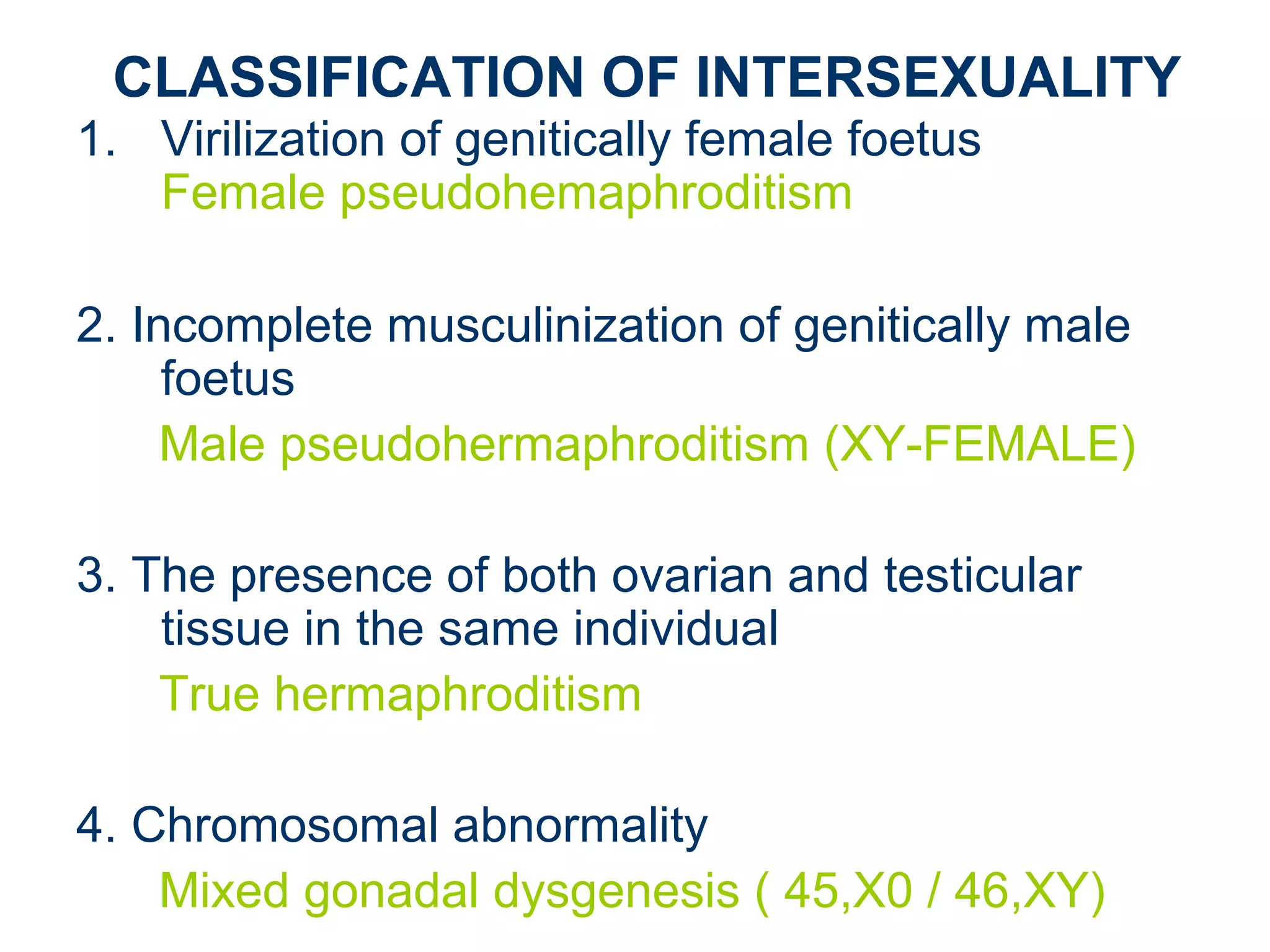
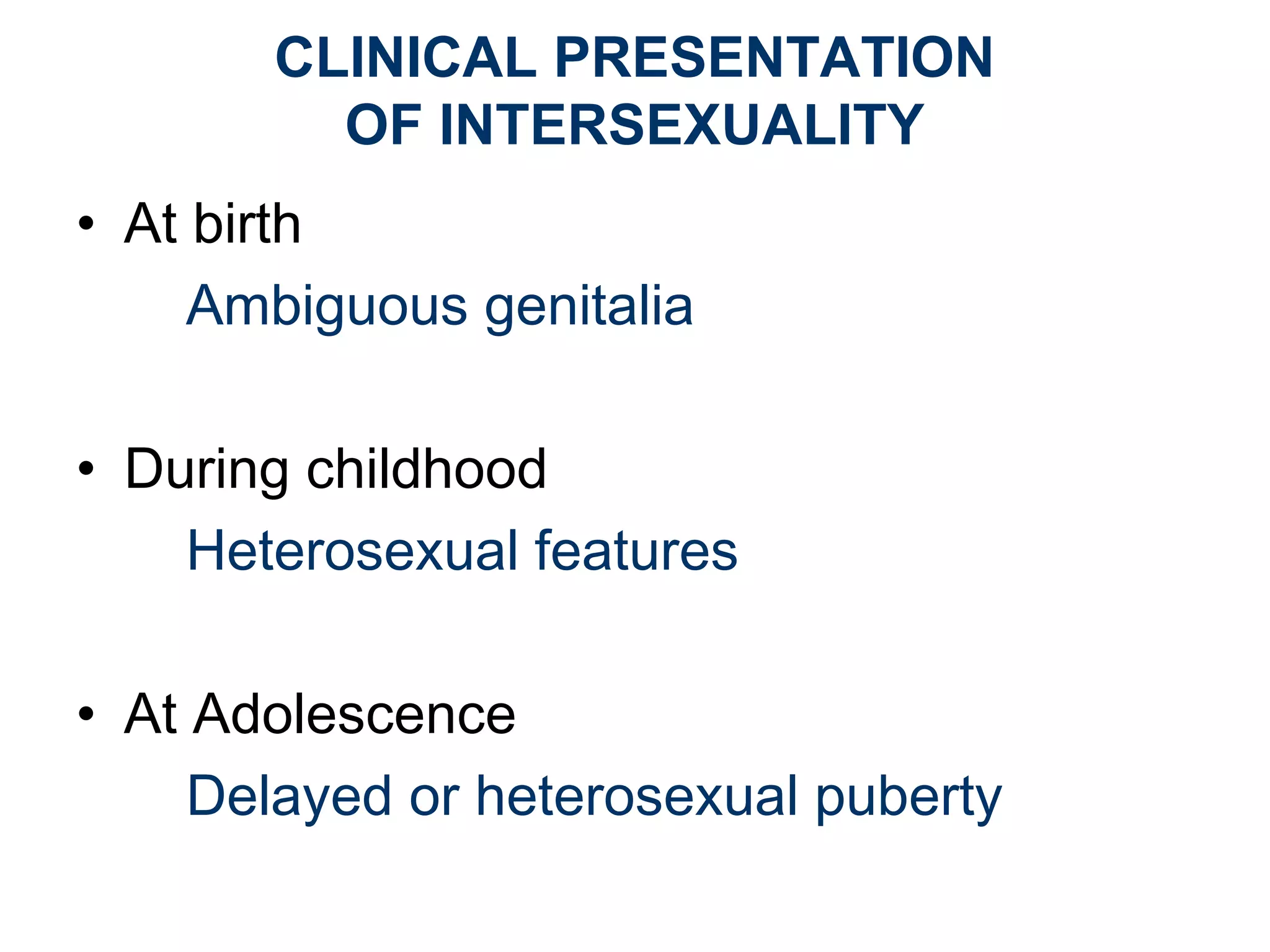
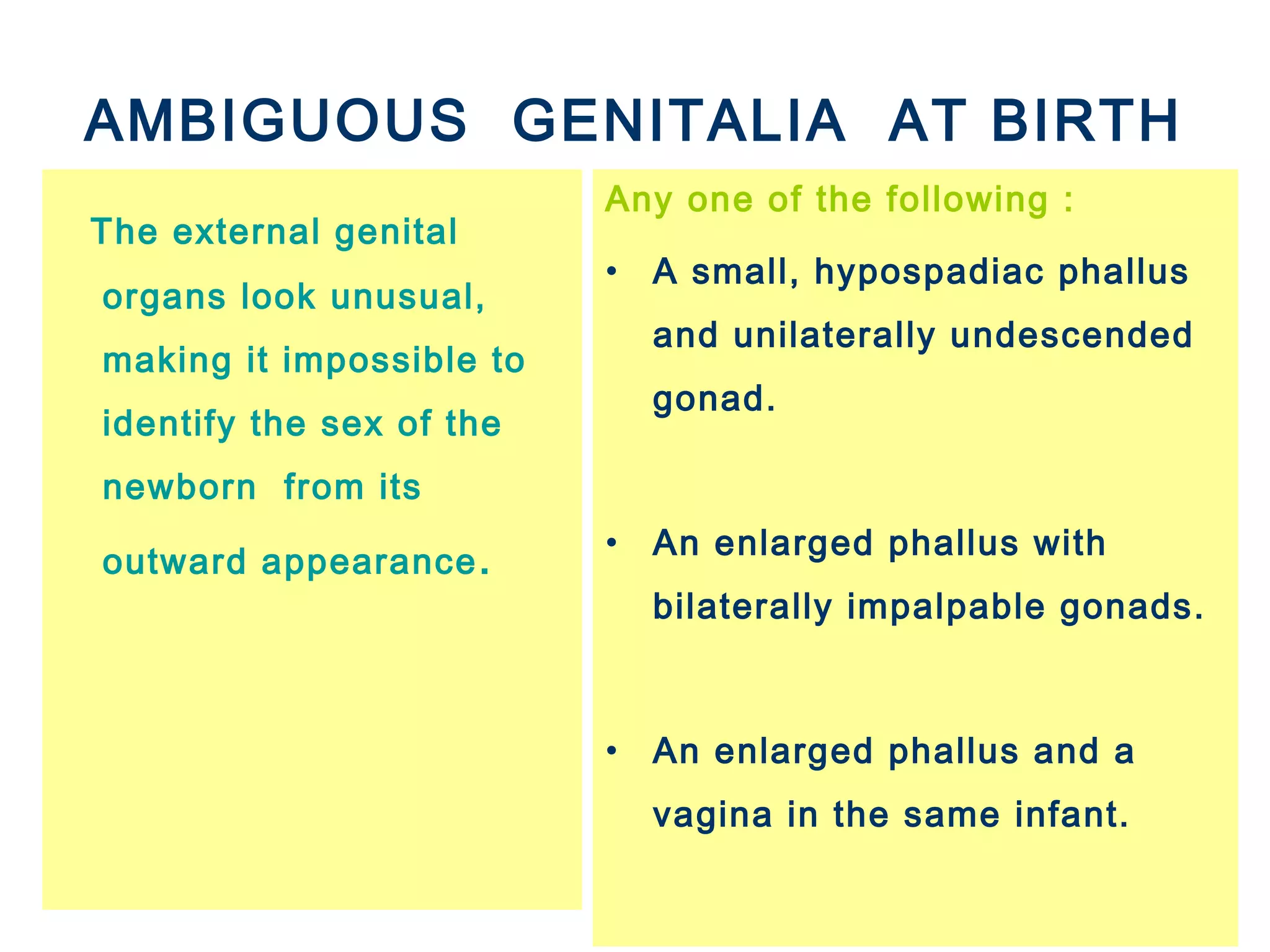
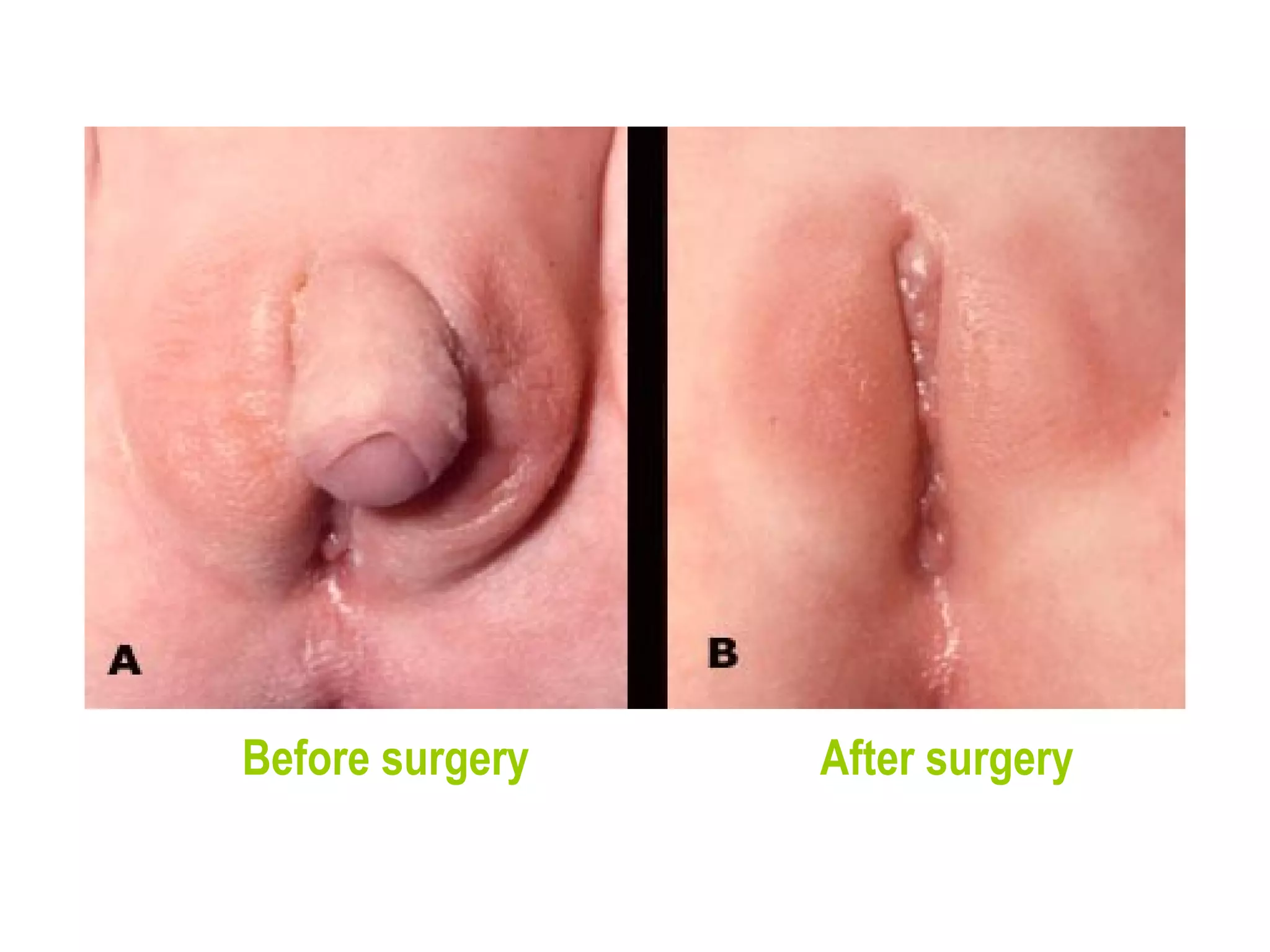
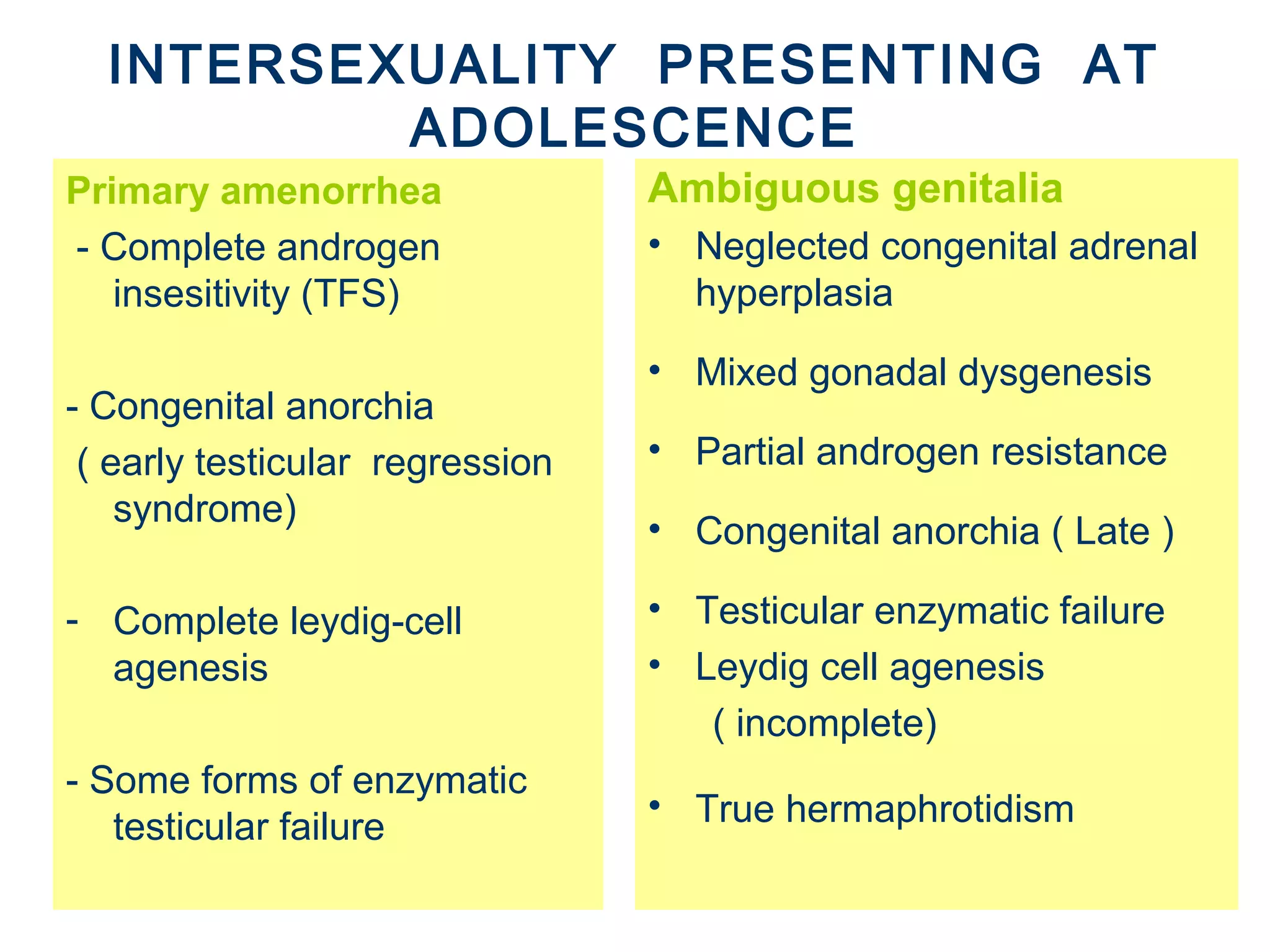
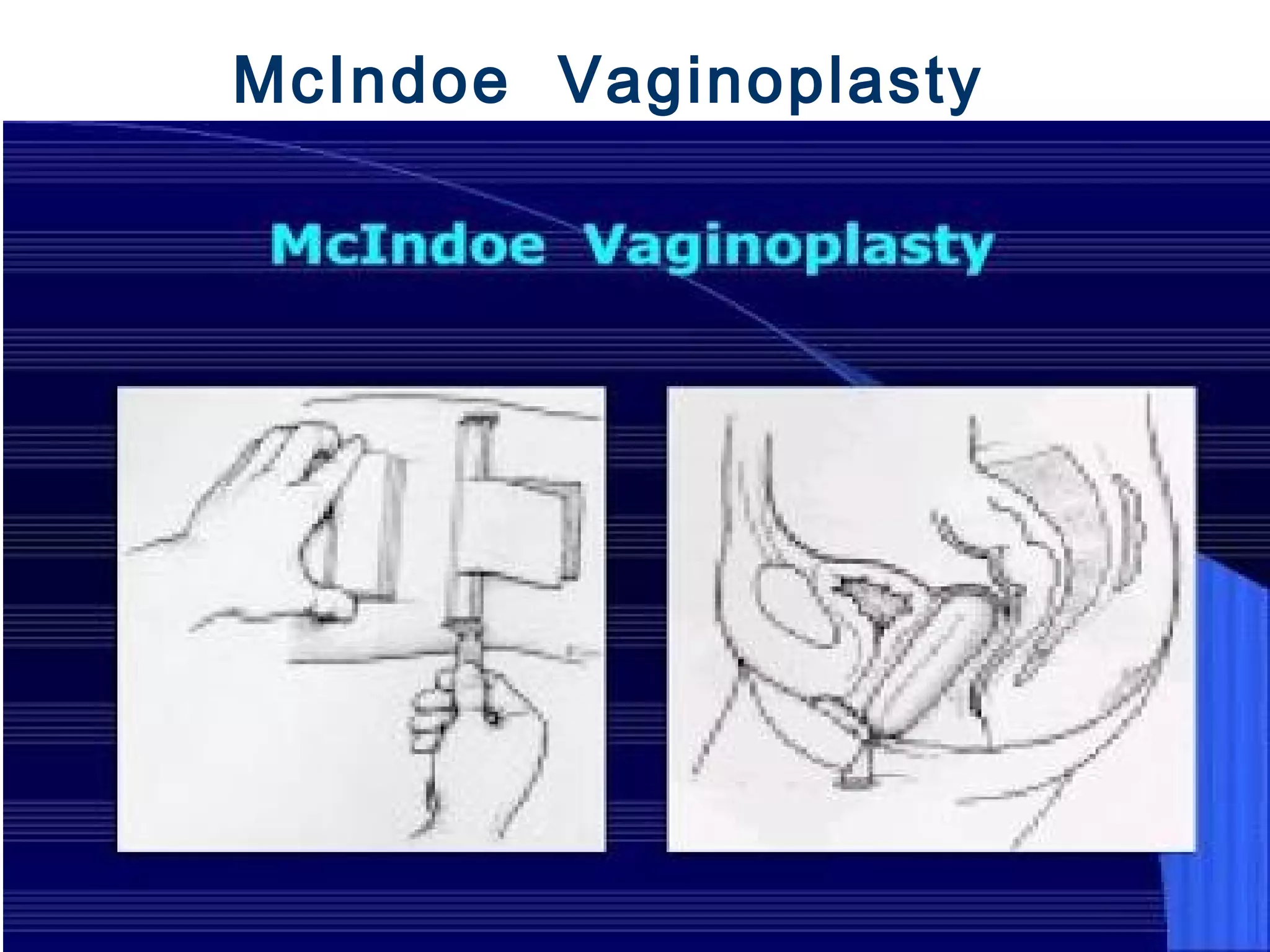
This document discusses the principles of managing ambiguous genitalia. It defines sex and gender, discusses human sexual differentiation and the classification of ambiguous genitalia. The key aspects of managing ambiguous genitalia in newborns include a thorough medical history, physical exam and investigations to determine sex assignment and any necessary surgical interventions. For adolescents presenting with intersex conditions, management may involve hormone replacement, corrective surgery, and maintaining or changing the individual's gender role based on diagnosis. A multidisciplinary team is important for properly diagnosing and treating individuals with intersex conditions at any age.