The document discusses various techniques used to measure intraocular pressure (IOP), including:
1) Digital tonometry which involves applying gentle pressure to the eyeball with a finger, though it is subjective.
2) Indentation tonometry like the Schiotz tonometer which measures corneal indentation from a known weight on a plunger, though readings require correction for ocular rigidity.
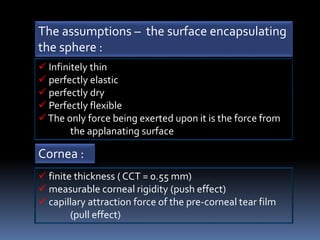
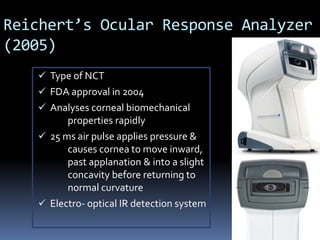
3) Applanation tonometry like the Goldmann tonometer which flattens a small corneal area to balance internal and external pressure, providing a more accurate IOP reading less influenced by ocular rigidity factors.