This document provides an overview of blood components and functions. It discusses:
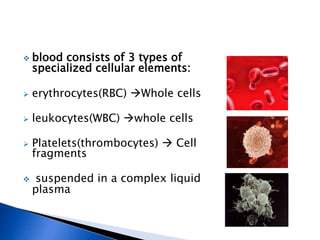
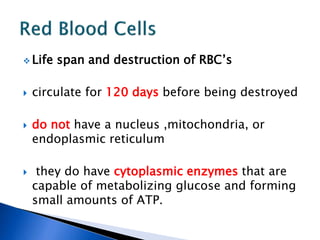
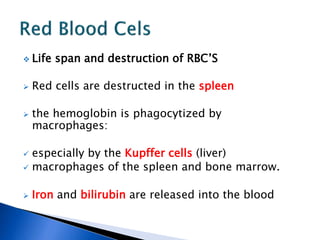
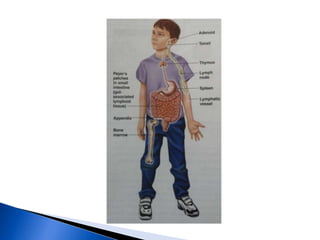
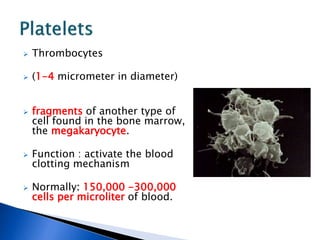
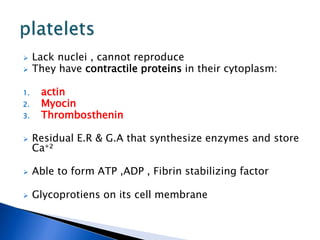
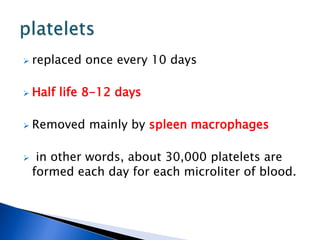
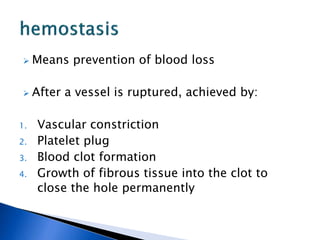
1. Blood consists of red blood cells, white blood cells, and platelets suspended in plasma.
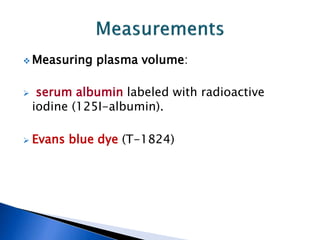
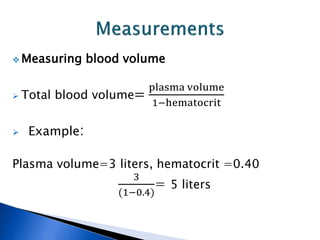
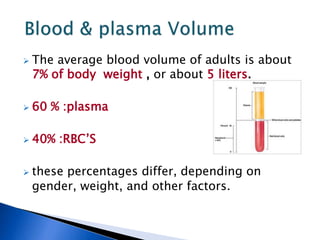
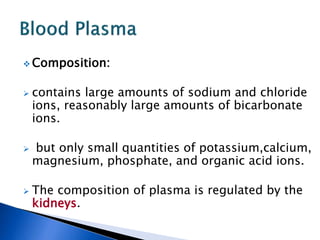
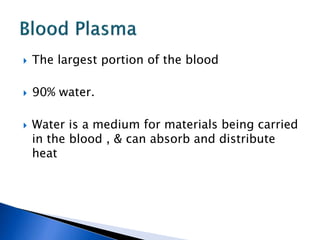
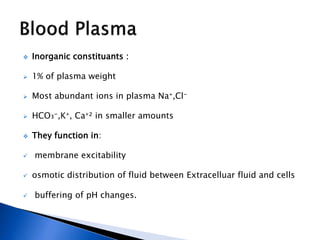
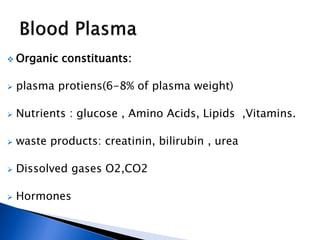
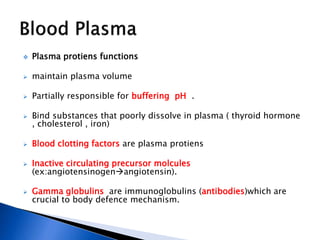
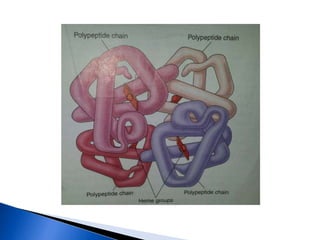
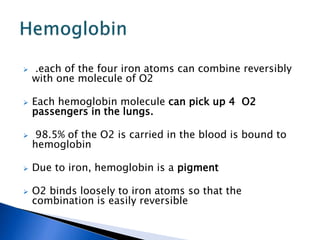
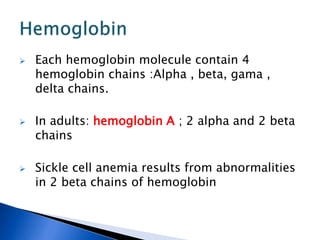
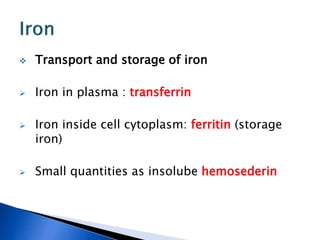
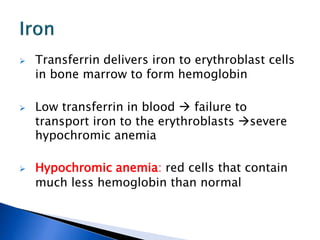
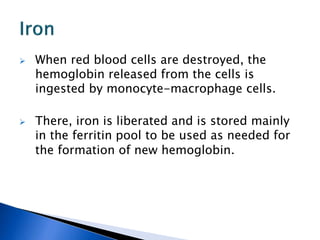
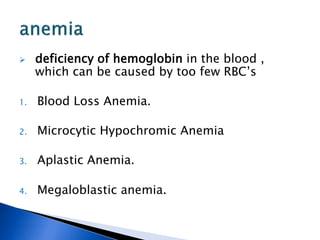
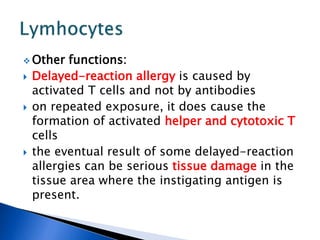
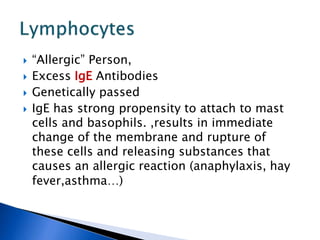
2. Plasma volume, blood volume, and the composition and functions of plasma and blood cells like hemoglobin, iron transport, and immune functions are described.
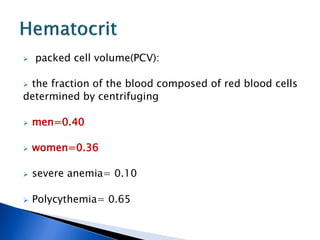
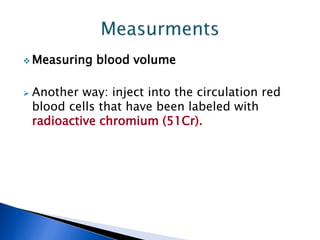
3. Measurement techniques for blood components like packed cell volume and blood volume are outlined.