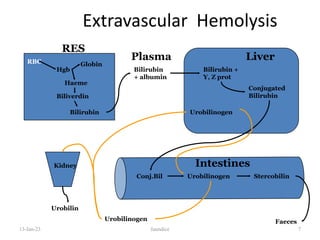
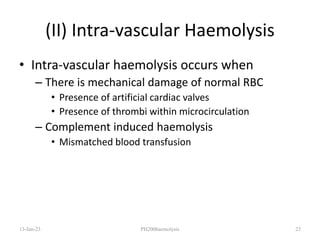
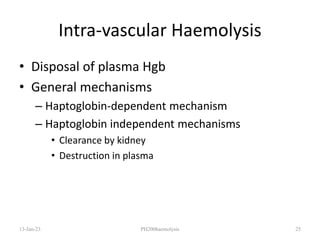
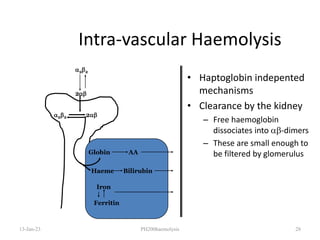
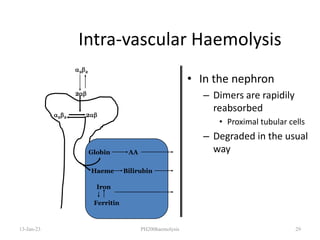
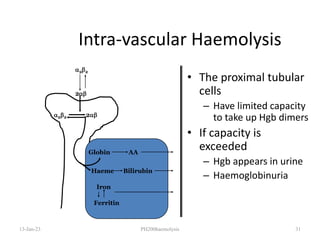
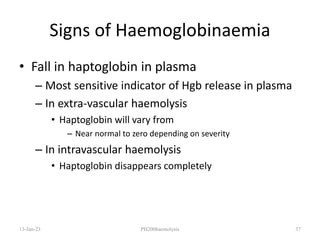
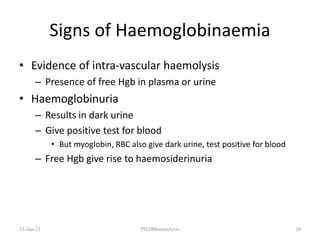
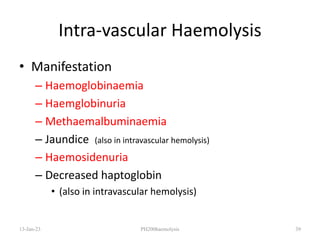
The document outlines the pathophysiology of haemolysis, characterized by the accelerated destruction of red blood cells (RBCs), which can occur due to various conditions such as renal failure and sickle cell disease. It distinguishes between intra-vascular and extra-vascular haemolysis, detailing the mechanisms of RBC destruction, bilirubin production, and compensatory responses in the bone marrow. Additionally, it discusses specific types of extra-vascular haemolytic anemia and the clinical manifestations associated with haemoglobin breakdown.