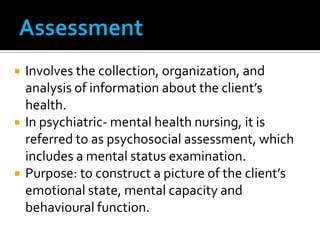
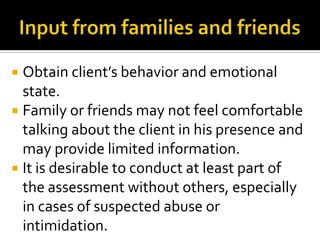
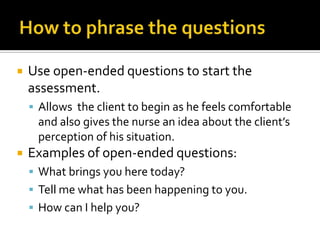
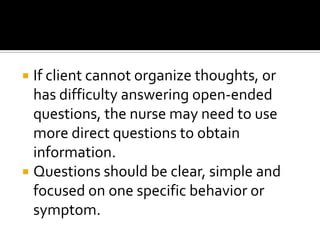
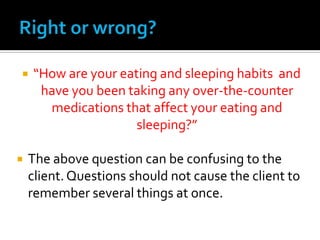
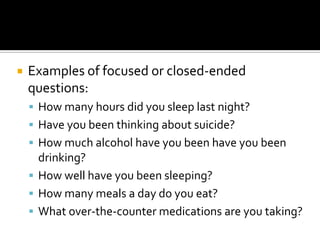
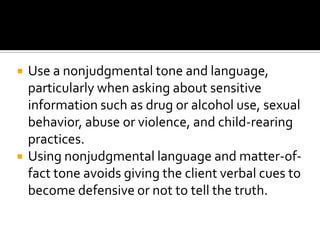
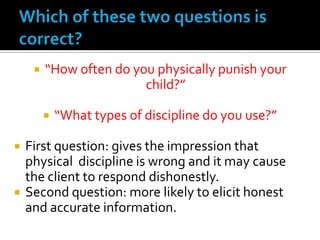
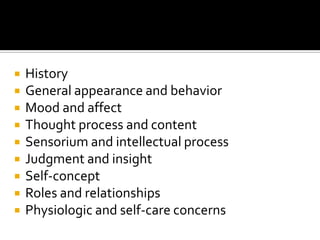
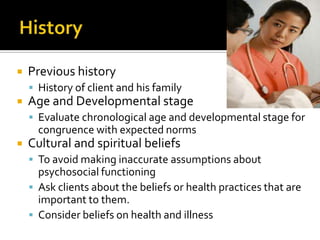
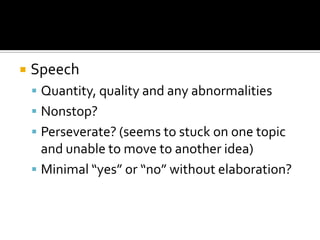
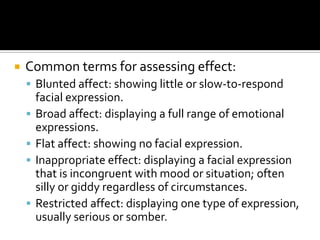
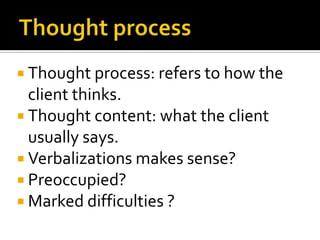
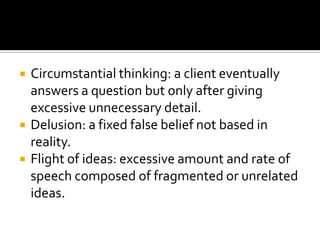
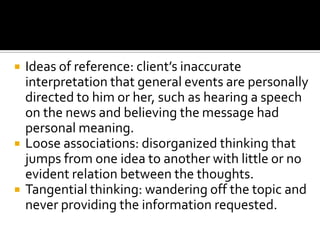
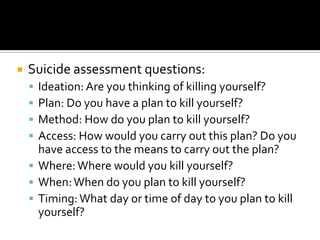
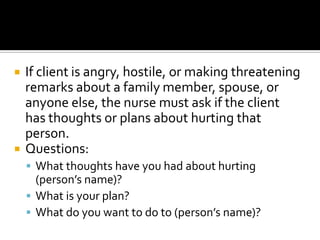
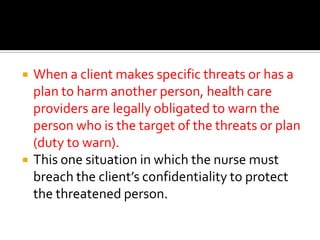
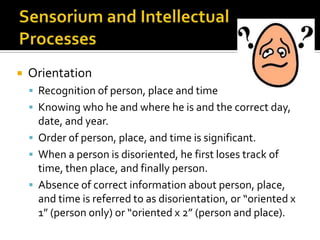
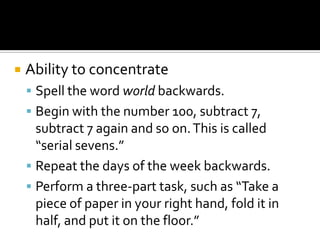
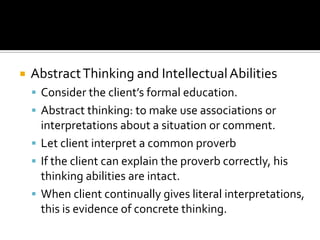
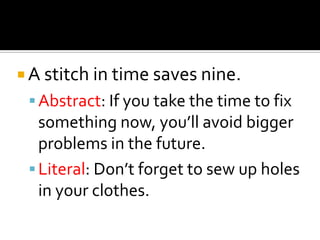
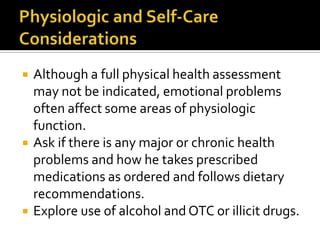
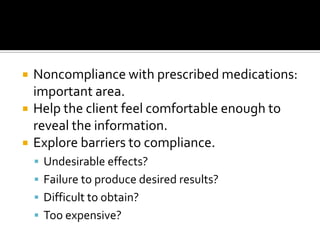
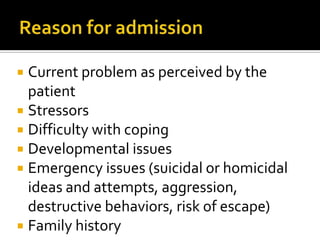
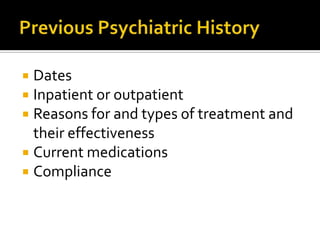
The document provides guidance on conducting a comprehensive psychosocial assessment in psychiatric nursing. It discusses key areas to assess including mental status, mood, thought process and content, cognition, risk of harm, relationships, and functioning. The nurse is advised to establish rapport, use open-ended and nonjudgmental questions, and assess for symptoms, stressors, strengths and risks to develop an accurate understanding of the client's situation.