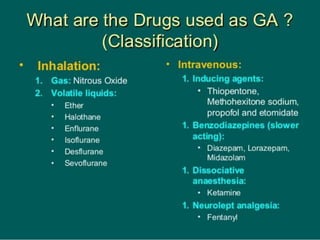
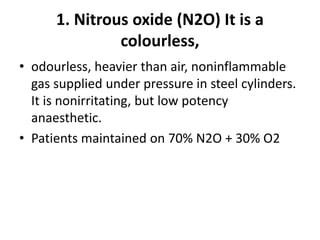
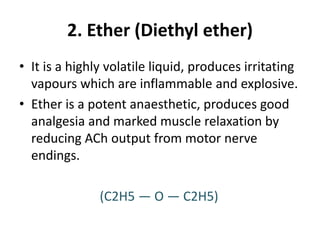
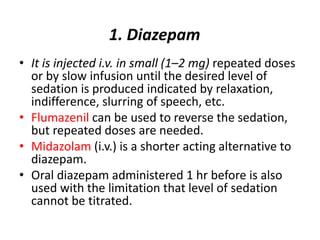
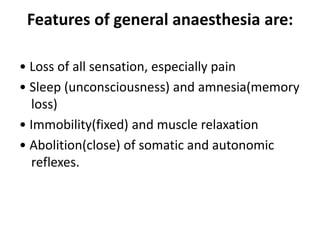
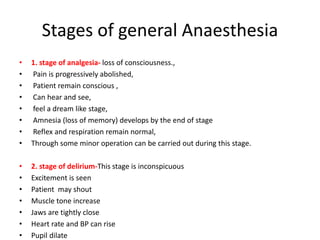
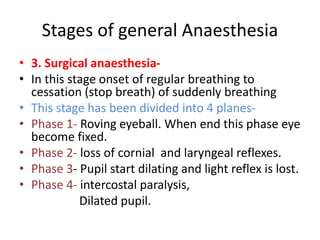
General anesthesia involves medications that induce unconsciousness during medical procedures. It uses a combination of intravenous drugs and inhaled gases to provide analgesia, amnesia, immobility and muscle relaxation while abolishing reflexes. There are four stages of general anesthesia - from initial analgesia and loss of consciousness to medullary paralysis where breathing and circulation cease. Inhalational anesthetics like nitrous oxide, halothane and isoflurane are administered via gas cylinders and machines and are eliminated primarily through exhalation. Intravenous drugs like thiopental and propofol are used for inducing and maintaining anesthesia while fentanyl and midazolam provide analgesia and sedation. Conscious sedation involves using these drugs at
![• Inhalational anaesthetics are gases or vapours that
diffuse rapidly across pulmonary alveoli and tissue
barriers.
• The depth of anaesthesia depends on the potency of
the agent,
• minimum alveolar concentration [MAC] is an index of
potency and its partial pressure (PP) in the brain,
• while induction and recovery depend on the rate of
change of PP in the brain.
• Transfer of the anaesthetic between lung and brain
• Alveoli Blood Brain](https://image.slidesharecdn.com/pptgeneralanasthesia-210127081731/85/General-anasthesia-9-320.jpg)