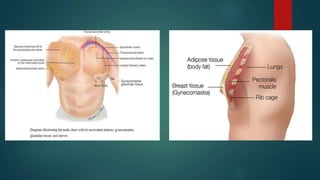
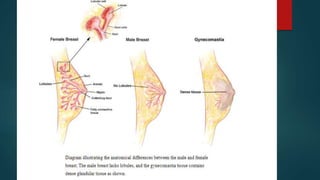
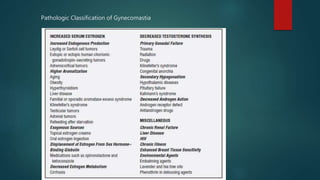
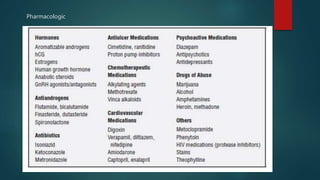
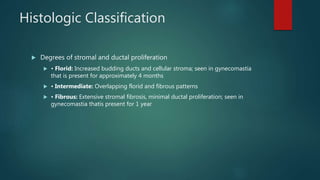
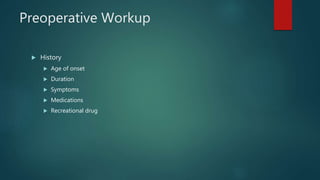
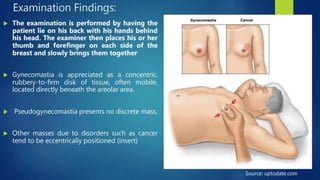
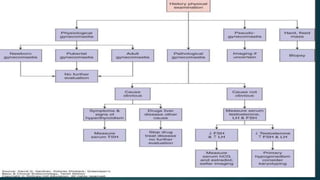
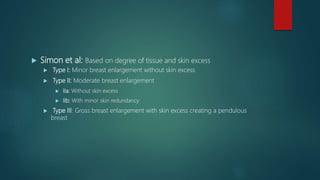
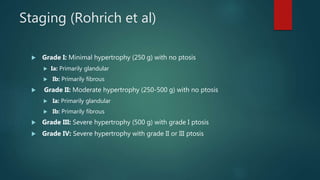
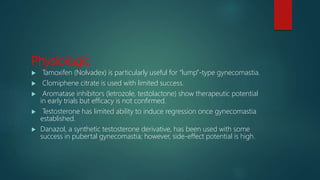
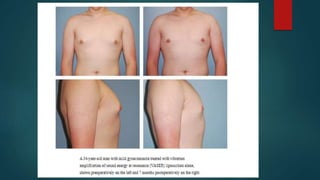
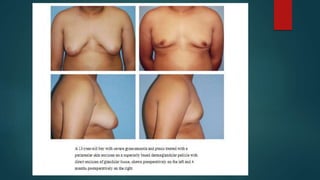
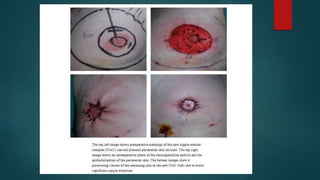
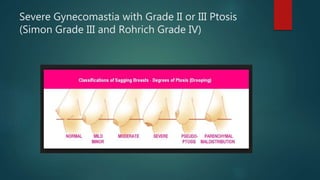
Gynecomastia refers to the benign enlargement of male breast tissue. It is a common condition, affecting up to 65% of adolescent boys. Causes include physiological changes during puberty or aging, as well as certain medications, medical conditions, or genetic factors. Diagnosis involves physical exam and sometimes lab tests or imaging to rule out other conditions. Treatment depends on severity but may include observation, medications to promote tissue regression, liposuction, or surgical excision of breast tissue. Surgical techniques aim to remove excess tissue while limiting scarring.