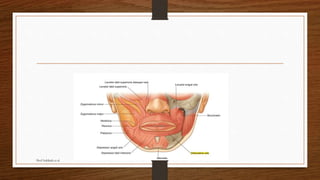
The document discusses various techniques for reconstructing defects of the lips after tumor resection, including:
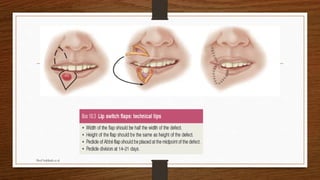
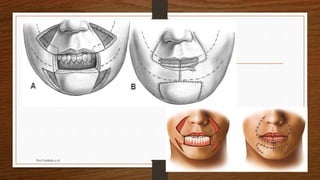
1. The Abbe-Estlander flap rotates tissue from the opposite lip to repair defects of over 30% of the upper or lower lip.
2. The Karapandzic flap mobilizes tissue from the lower nasolabial region to reconstruct large lower lip defects.
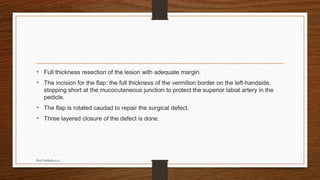
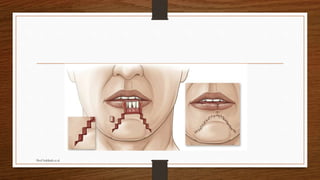
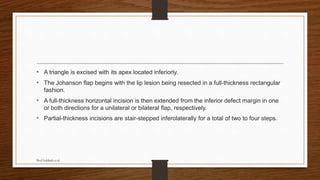
3. The Johanson step ladder advancement flap excises small rectangles from the sides of the lower lip defect to close gaps.
It also describes techniques for reconstructing the vermilion border and commissures, as well as complications of lip reconstruction.