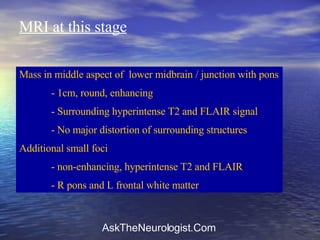
A 56-year-old Syrian woman presented with progressive brainstem and frontal syndrome symptoms. MRI showed a lesion in the lower midbrain along with smaller subcortical lesions. She developed coma but recovered consciousness with steroids, though remained with severe frontal deficits. The clinical picture is best explained by granulomatous angiitis of the nervous system.