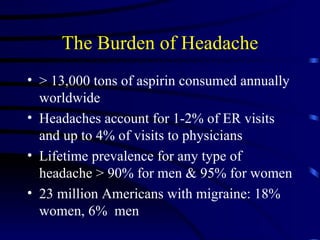
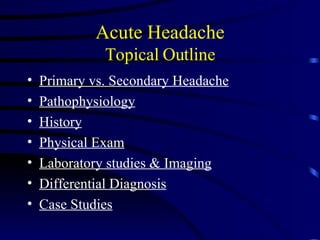
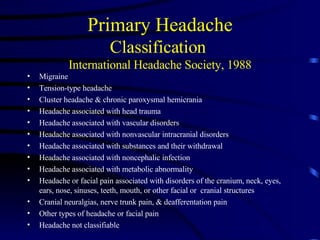
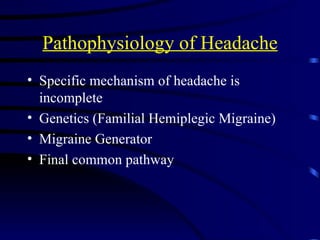
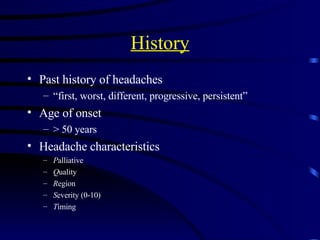
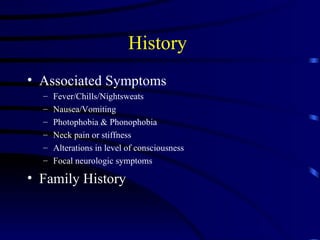
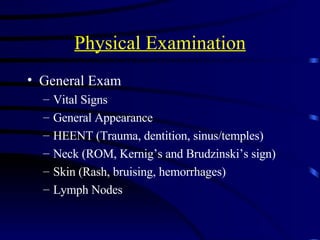
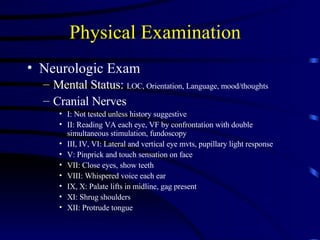
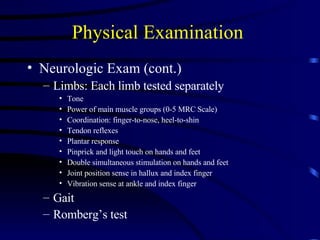
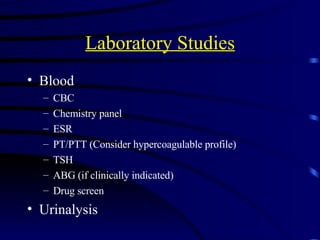
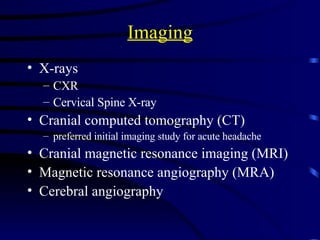
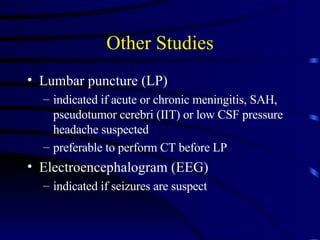
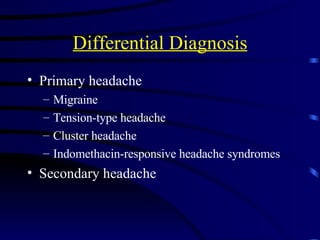
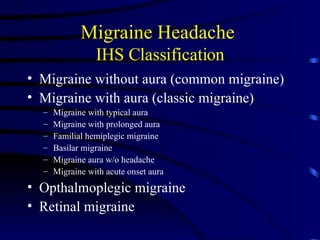
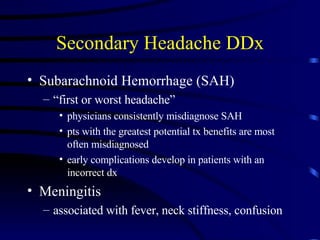
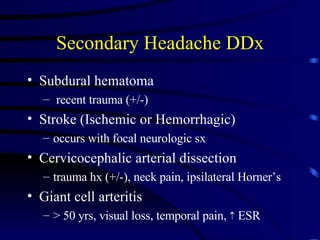
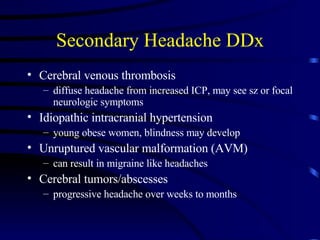
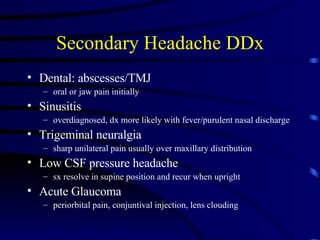
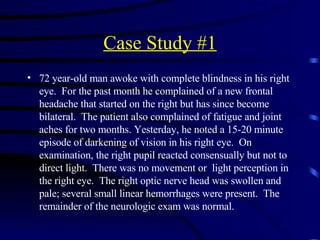
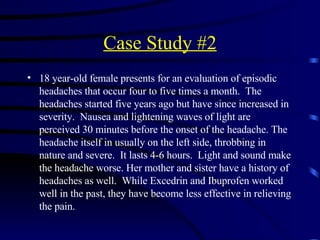
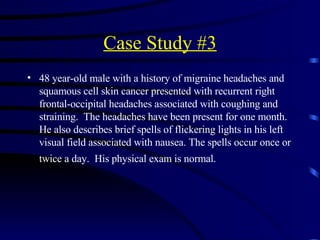
This document provides an overview of acute headaches. It begins with background on the burden of headaches worldwide. It then outlines the topics to be covered including the difference between primary and secondary headaches, pathophysiology, history and exam findings, diagnostic studies, differential diagnosis, and case studies. Key points are that headaches are common, migraines and tension-type headaches are primary headache types, and secondary headaches can indicate underlying conditions like subarachnoid hemorrhage that require prompt diagnosis and treatment.