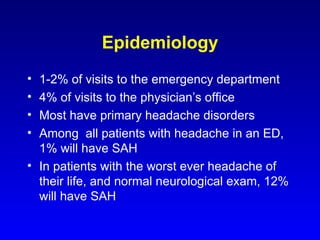
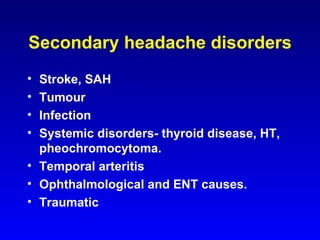
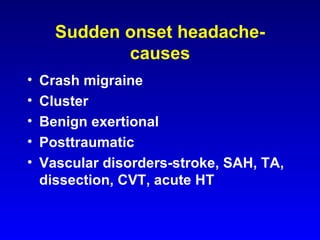
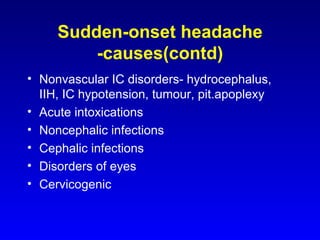
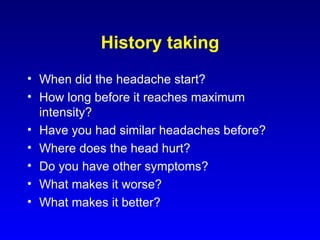
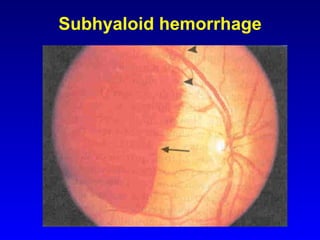
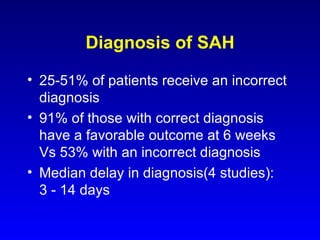
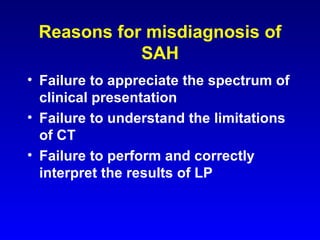
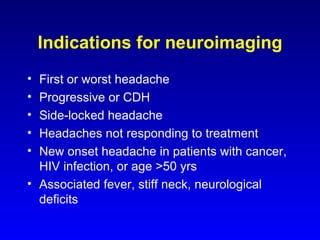
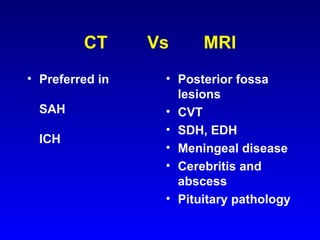
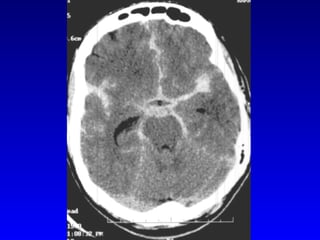
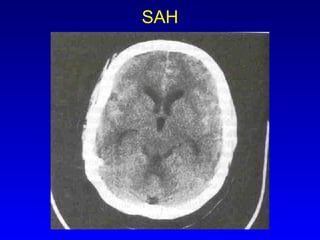
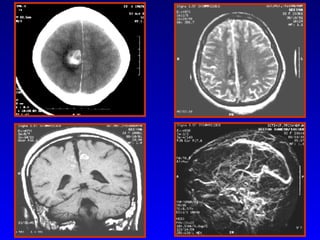
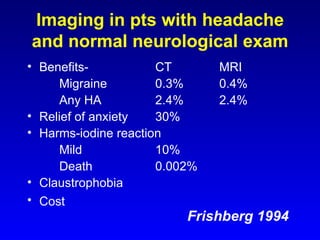
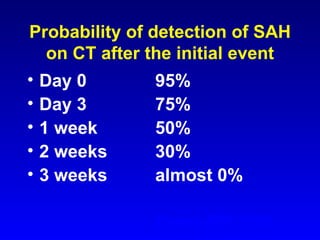
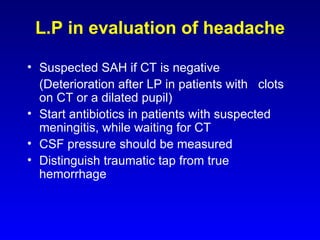
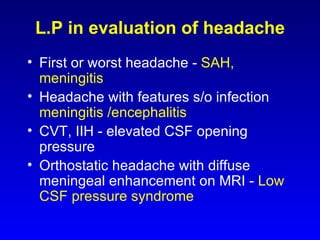
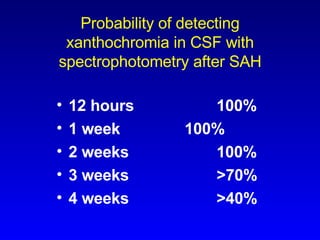
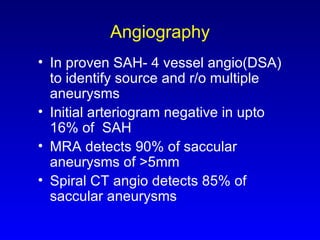
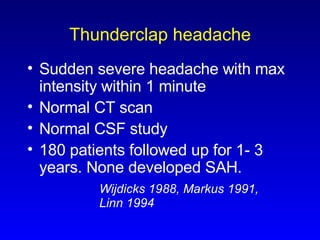
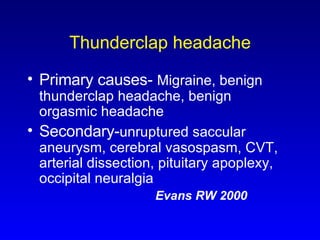
The document discusses sudden onset headaches, providing information on epidemiology, causes, evaluation, diagnosis, and management. It notes that sudden onset headaches can be caused by primary headache disorders like migraine or secondary causes like stroke, subarachnoid hemorrhage (SAH), and tumors. A thorough history and physical exam are important, and imaging like CT or MRI along with lumbar puncture may help diagnose conditions like SAH. Proper diagnosis is key as misdiagnosis can lead to worse outcomes.