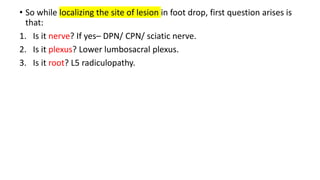
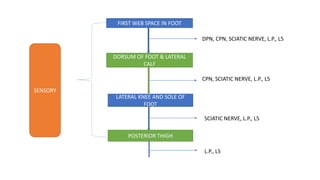
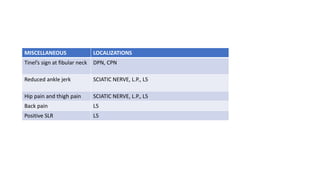
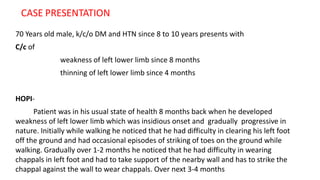
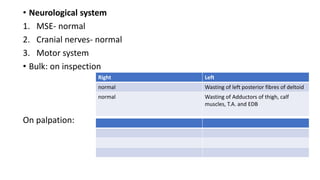
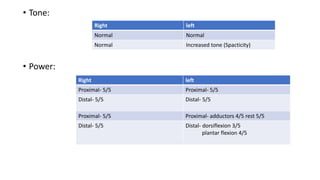
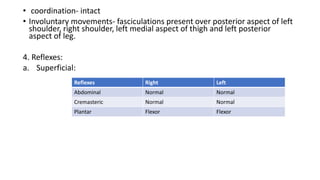
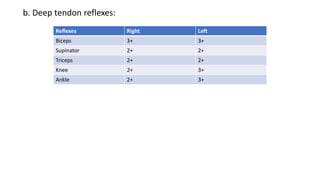
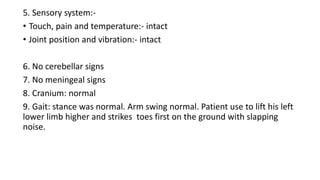
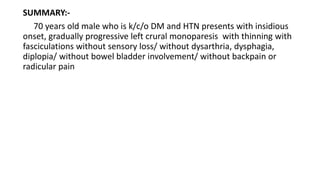
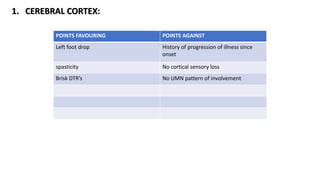
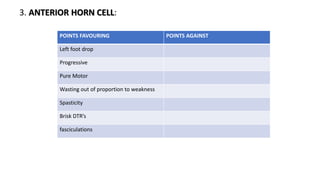
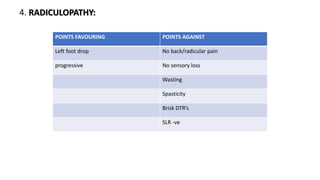
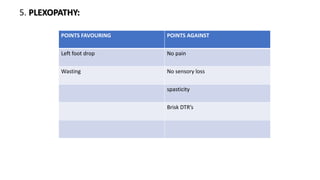
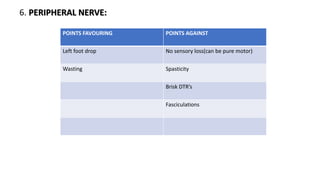
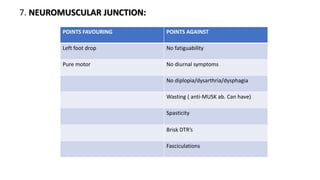
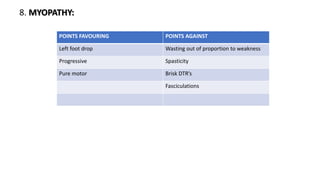
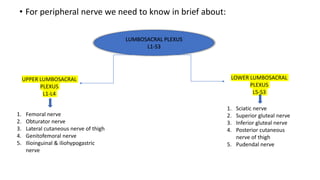
A 70-year-old male with a history of diabetes and hypertension presents with insidious onset and progressive weakness and thinning of the left lower limb, with no sensory loss or other neurological symptoms. Clinical examination reveals left lower limb weakness and fasciculations, indicating possible causes ranging from anterior horn cell pathology to peripheral nerve involvement. The document discusses localization of foot drop symptoms and the relevant anatomical considerations for the sciatic nerve and its branches.
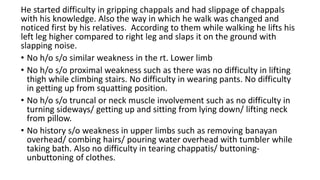

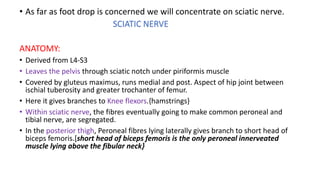
![• Above the popliteal fossa the sciatic nerve physically bifurcates into
common peroneal nerve and tibial nerve.
• Common peroneal nerve first gives rise to lateral cutaneous nerve of
knee then it winds around fibular neck and then divides into
DEEP PERONEAL NERVE
MOTOR:
• Dorsiflexors of
foot and
toes[TA, EHL,
EDL, EDB]
• Peroneus
tertius
SENSORY:
• First web
space.
SUPERFICIAL PERONEAL NERVE
MOTOR:
• Ankle
evertors{P.L.&
P.B.}
SENSORY:
• Mid and lower
lateral calf.
• Dorsum of foot
and dorsal
medial 3 or 4
toes upto IPJ.](https://image.slidesharecdn.com/footdrop-220618064551-73e84025/85/Approach-to-foot-drop-25-320.jpg)