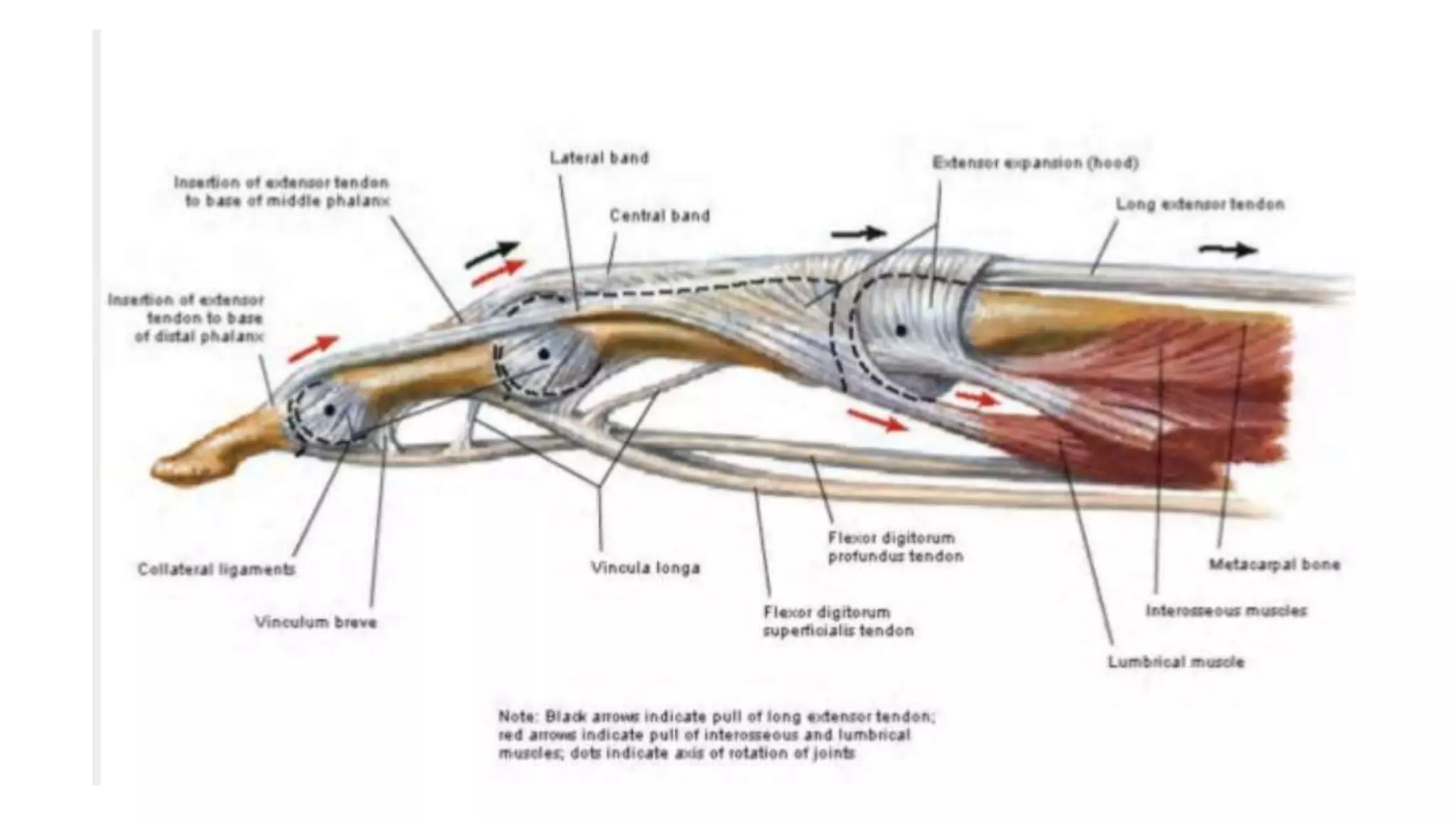
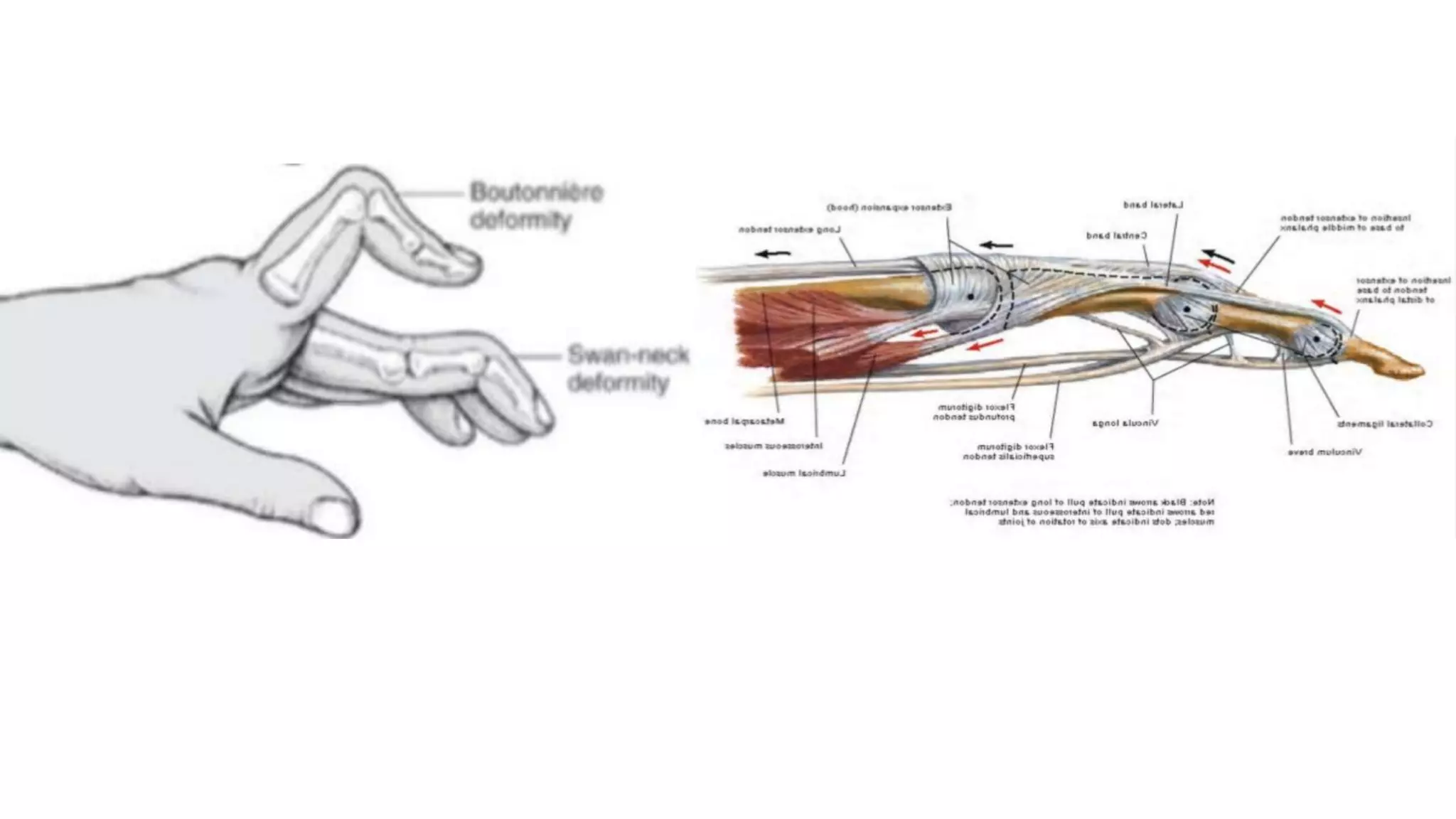
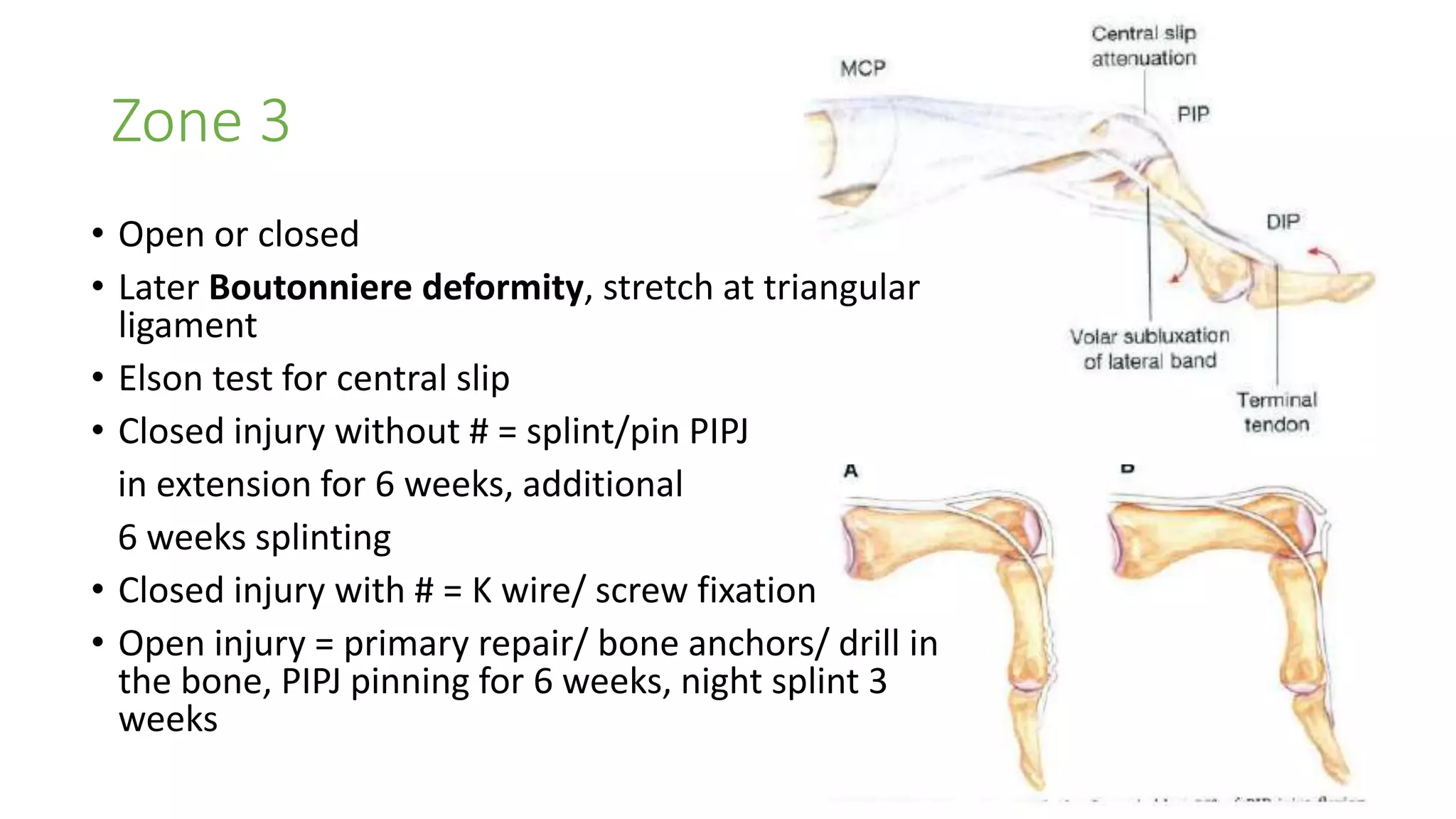
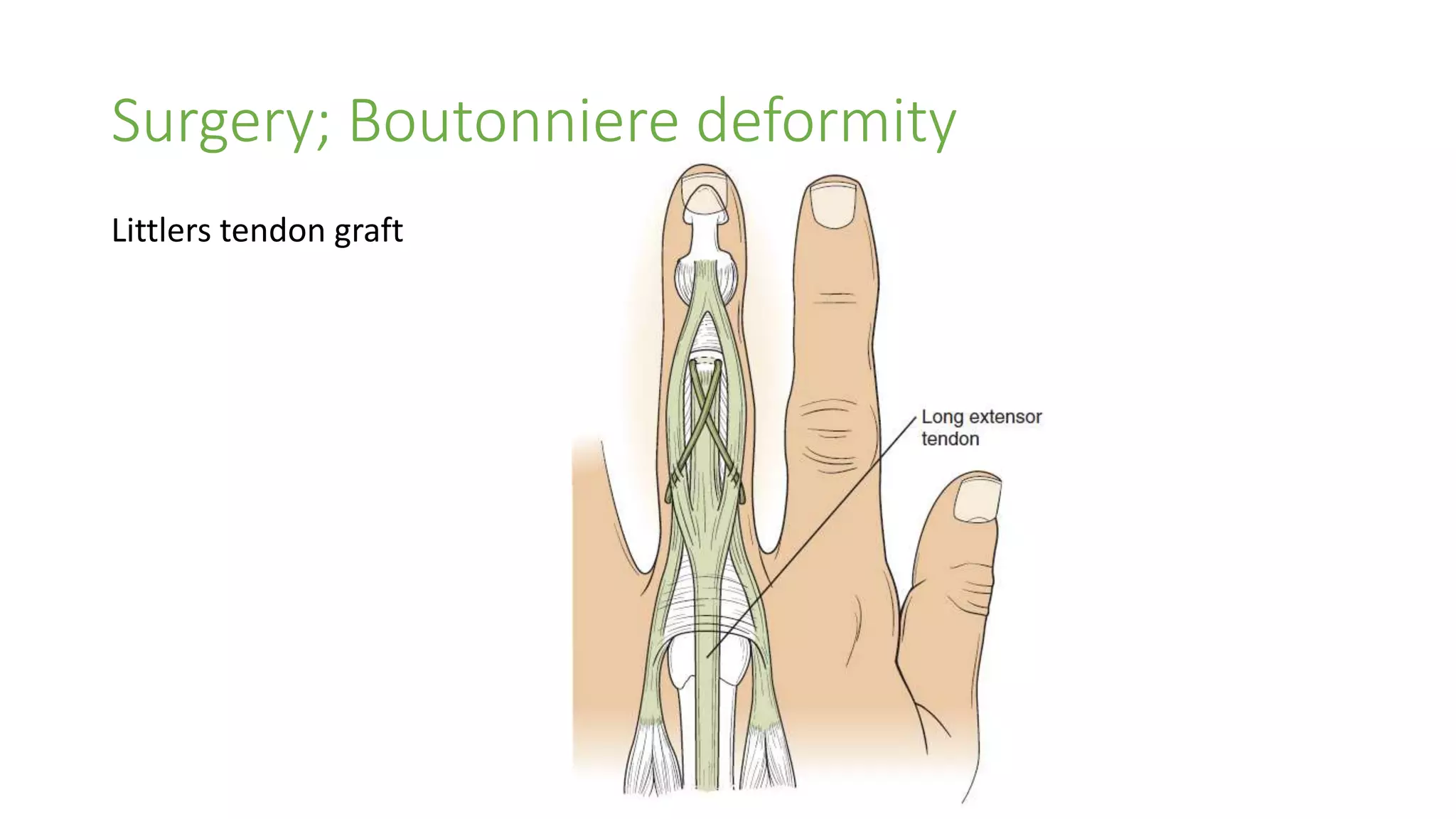
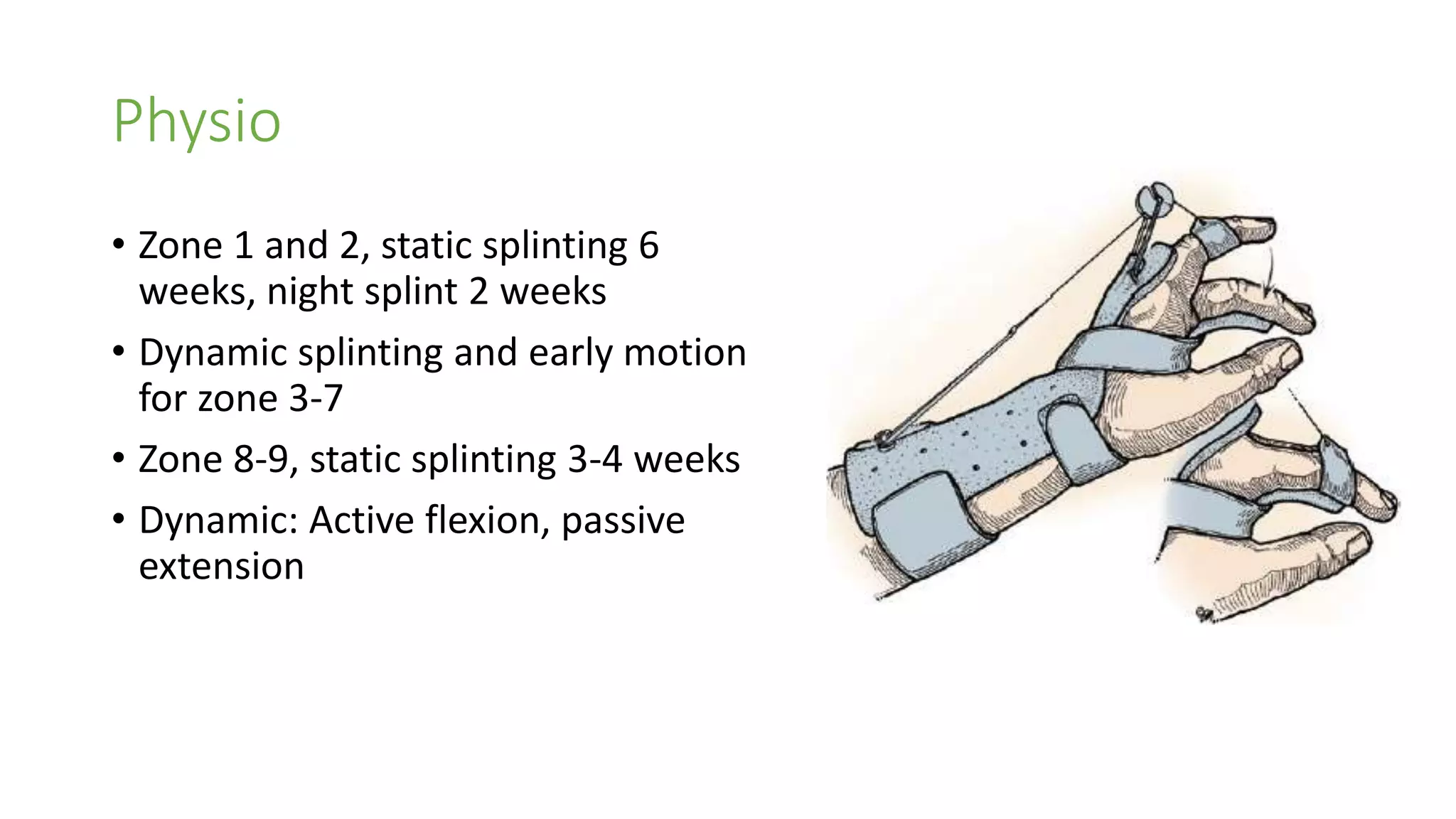
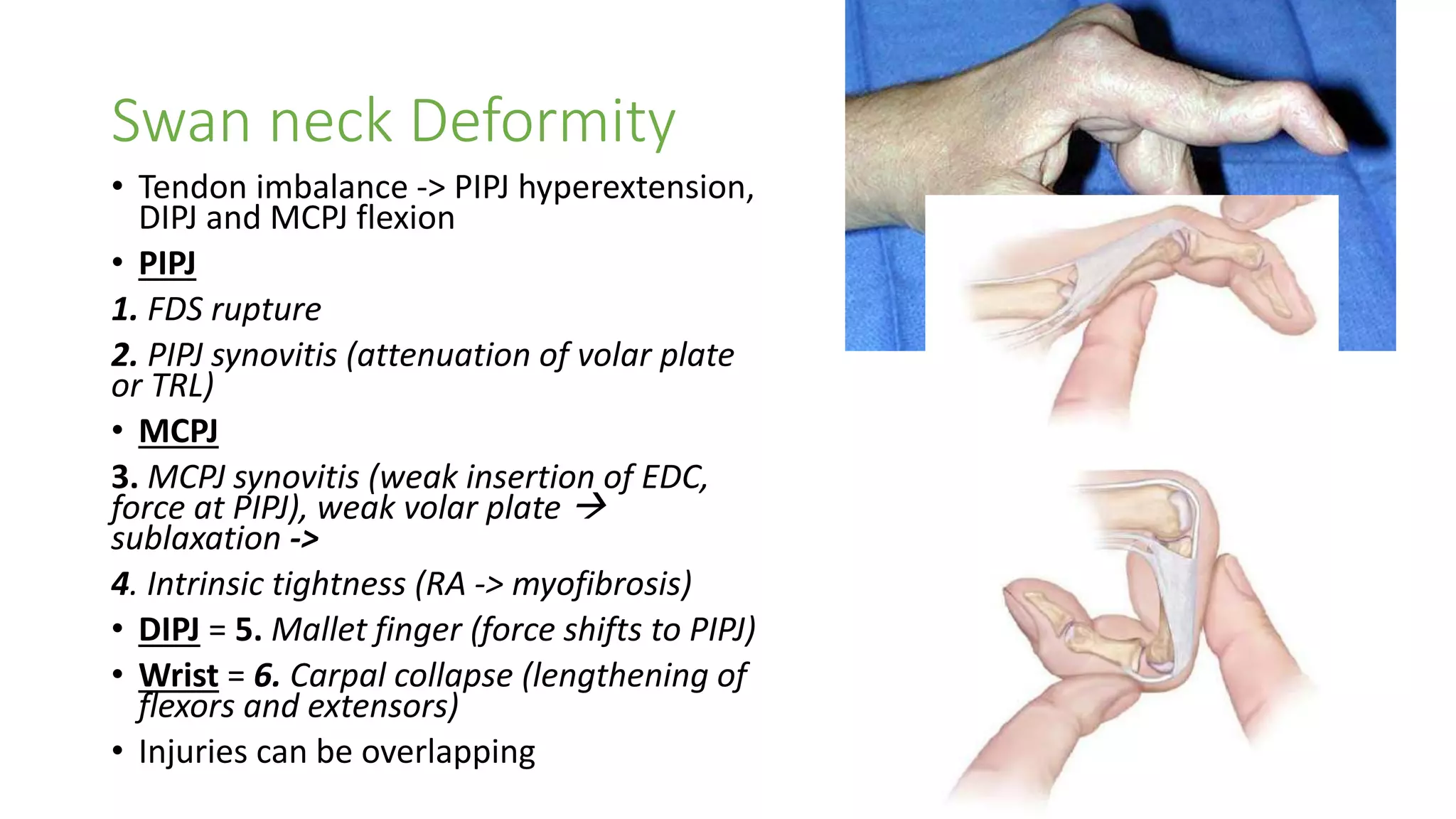
This document summarizes different types of extensor tendon injuries and their treatment. It discusses mallet finger injuries, describing 4 types and their respective treatments which may include splinting or surgical repair. It also covers Boutonniere deformity, its causes, and potential surgical treatments like Fowler tenotomy or Littler tendon graft. Finally, it outlines different injury zones 1-9, from the DIP joint to the muscle belly, and recommendations for treatment including splinting, suturing, or tendon repair depending on the specific zone and nature of the injury.