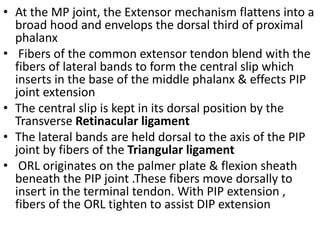
1. The extensor mechanism of the fingers consists of the central slip and lateral bands which insert at various joints to extend the fingers.
2. Injuries can occur in different zones from the DIP to the forearm. Zone I injuries occur at the DIP joint while zone II injuries involve the lateral bands.
3. Boutonniere deformities result from zone III injuries where the central slip is disrupted. Management depends on the chronicity and flexibility of the deformity.