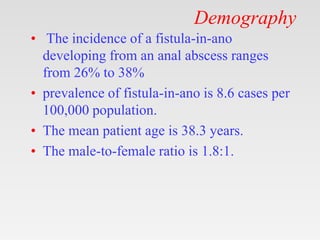
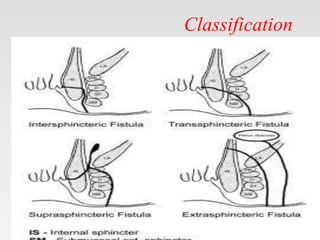
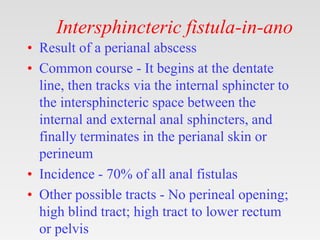
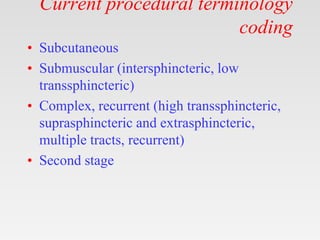
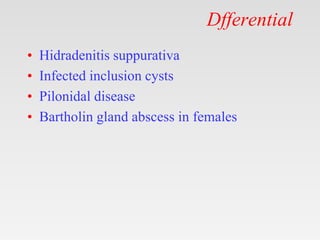
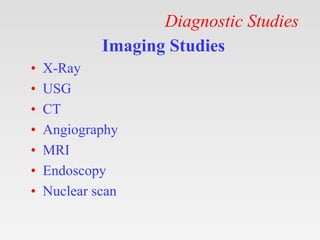
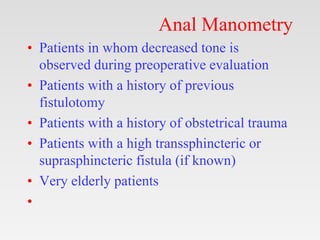
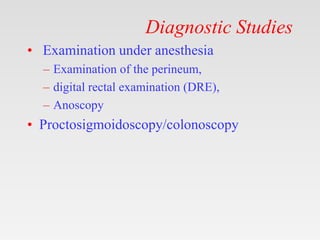
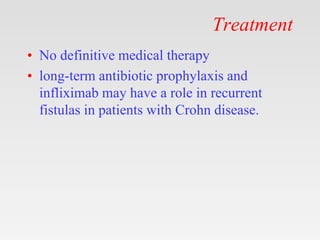
This document provides tips and instructions for using a PowerPoint presentation on fistula-in-ano. It recommends presenting blank slides to students and asking them questions to promote active learning. The PowerPoint covers topics like definition, anatomy, etiology, classification, clinical features, investigations, and management of fistula-in-ano over multiple revisions for learning. It also provides links to view and download the full PowerPoint presentation.