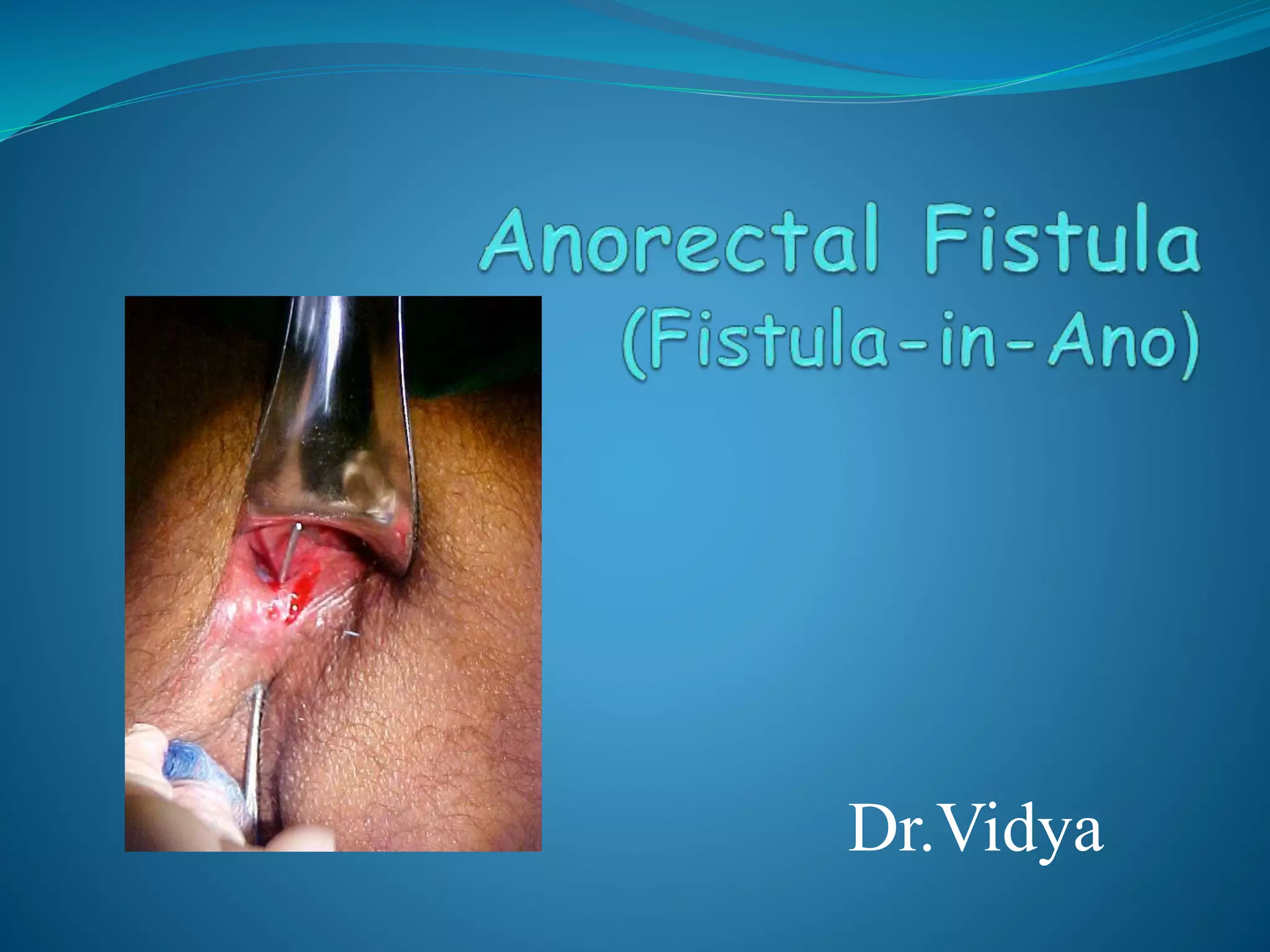
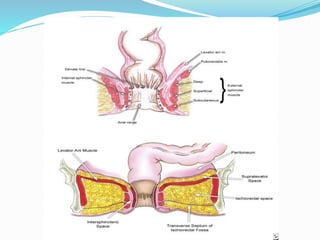
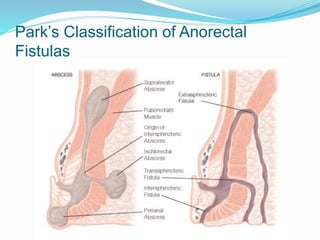
1) Anorectal fistulas are abnormal connections between the anal canal and perianal skin that usually form after an anorectal abscess bursts spontaneously.
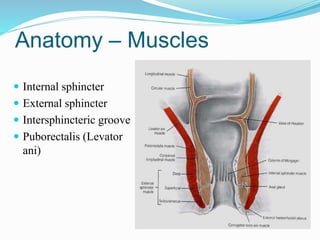
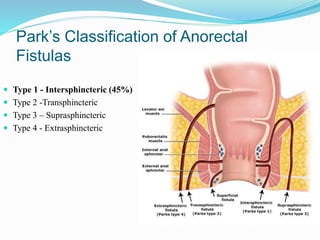
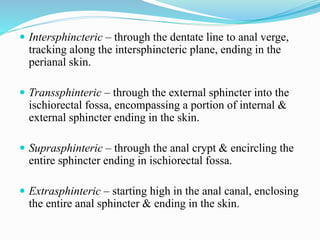
2) Park's classification system categorizes fistulas as intersphincteric, transphincteric, suprasphincteric, or extrasphincteric based on their path through the anal sphincter muscles.
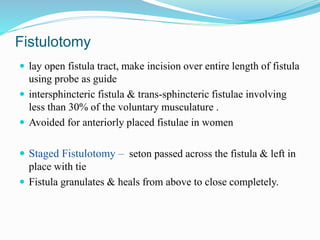
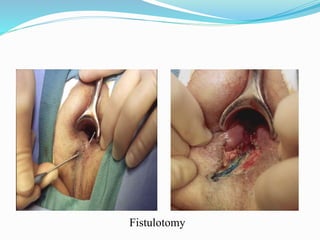
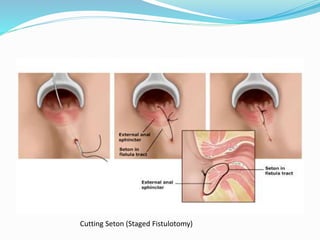
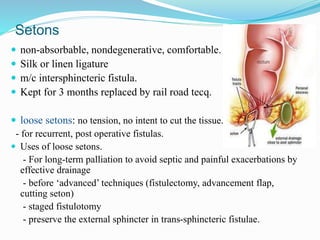
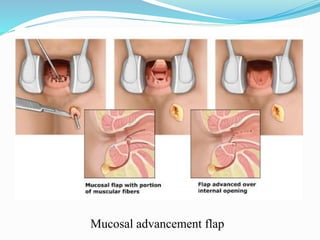
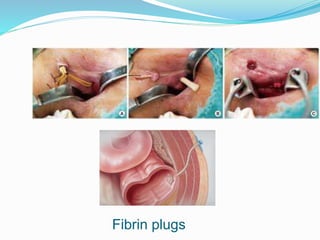
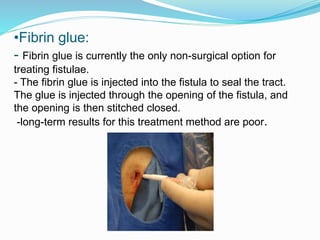
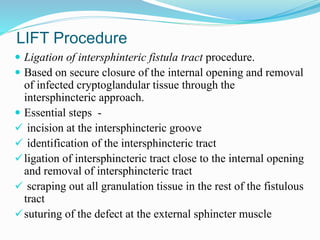
3) Treatment options include fistulotomy, seton placement, advancement flaps, fibrin plugs, and the LIFT procedure. The goal is to drain infection and eradicate the fistula tract while preserving sphincter function and avoiding recurrence.