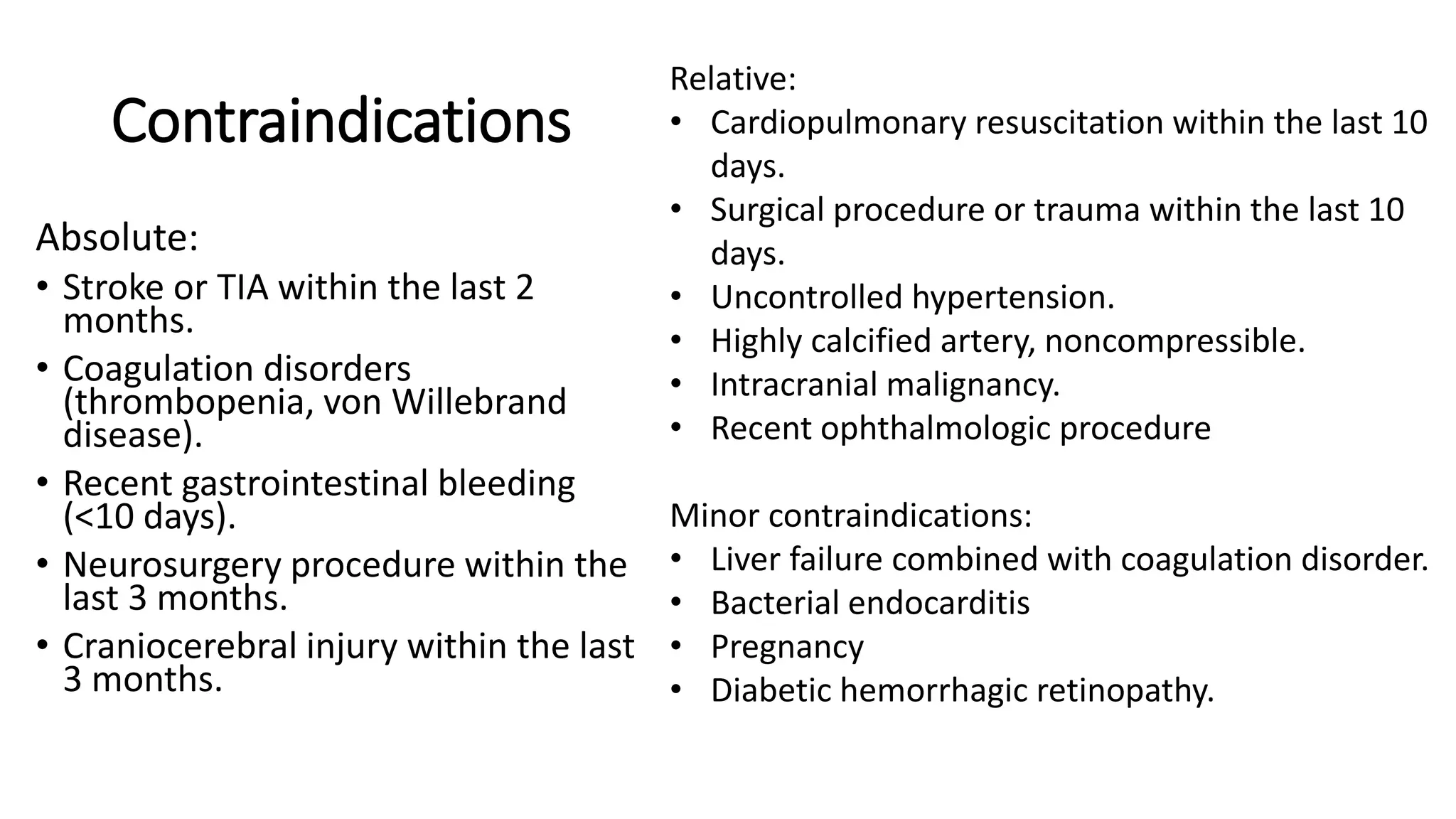
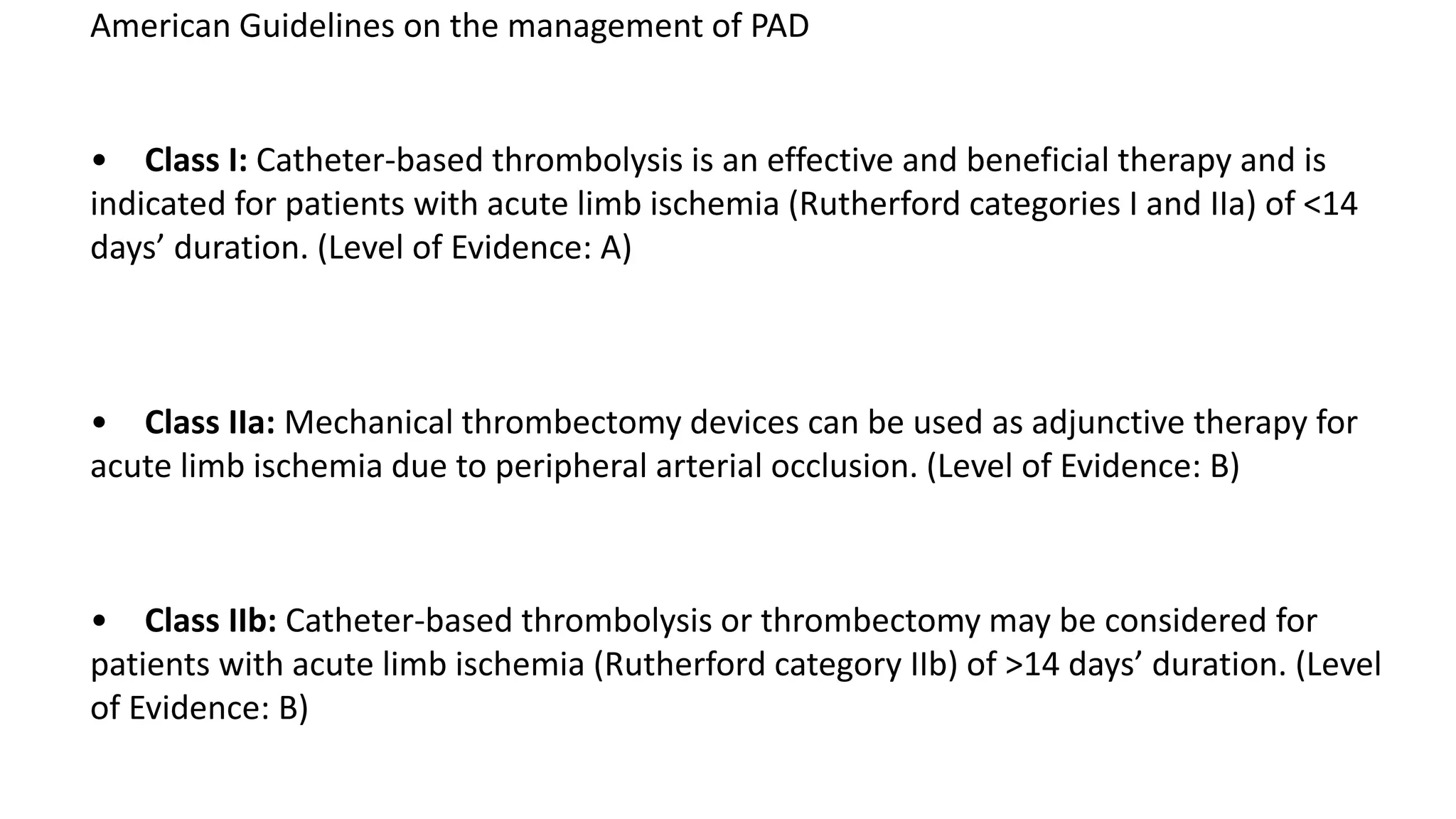
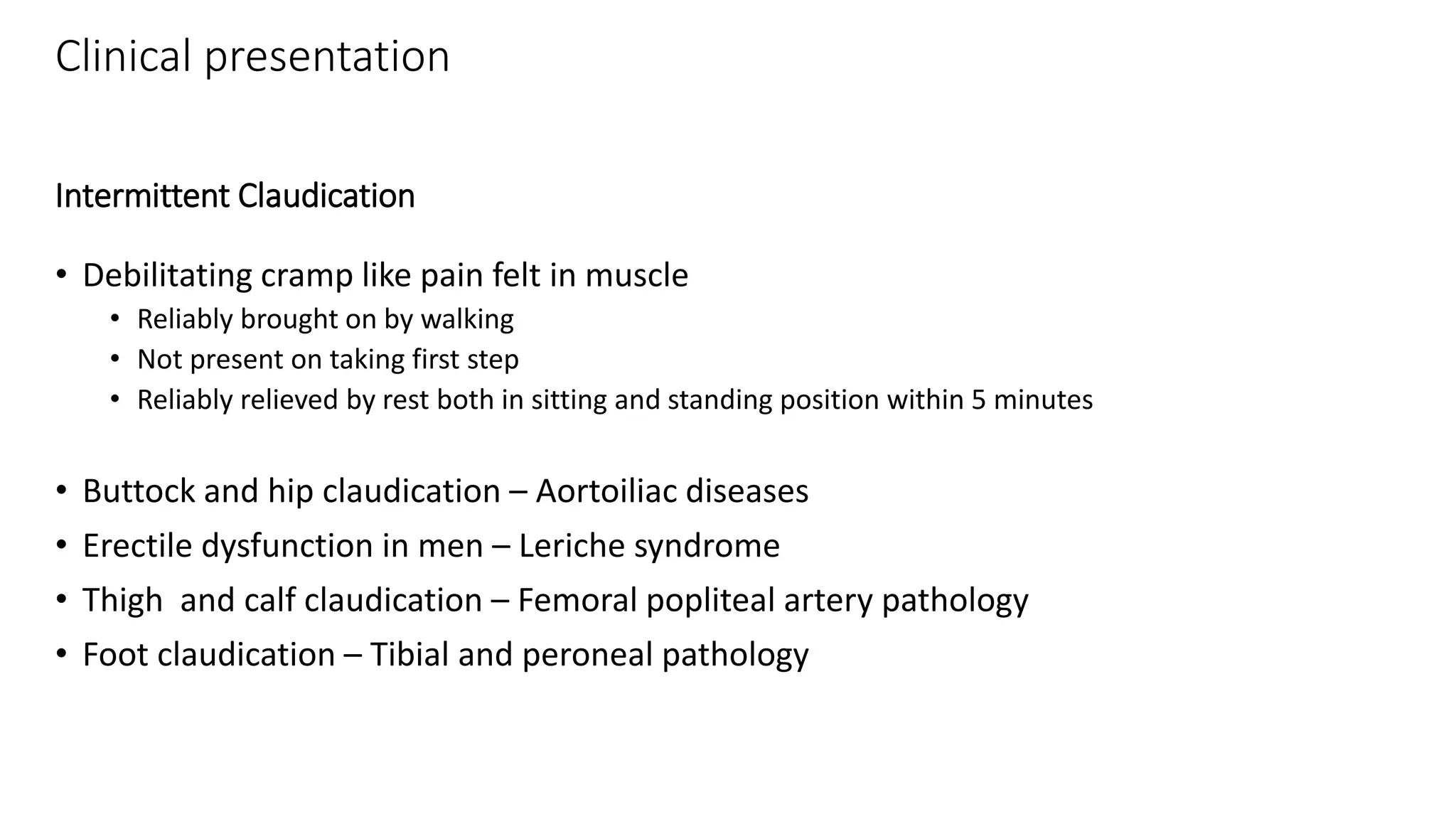
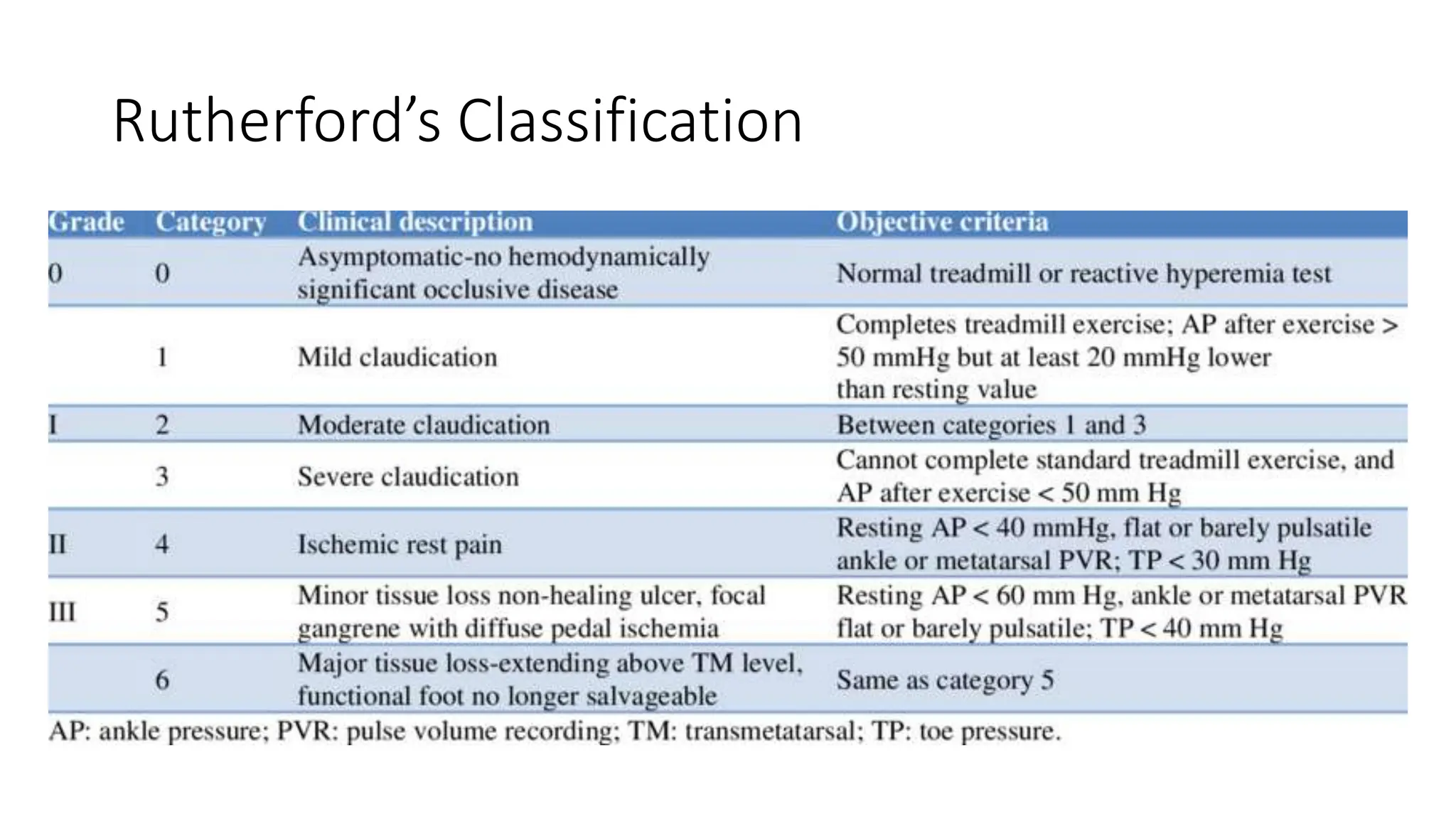
This document provides an overview of peripheral arterial disease (PAD), including its clinical presentations and management. PAD is caused by atherosclerosis obstructing arteries other than those supplying the heart or brain. It most commonly presents as intermittent claudication, or leg pain with walking that resolves with rest. Diagnosis involves ankle-brachial pressure index testing, imaging studies like duplex ultrasound, CT or MR angiography. Treatment focuses on risk factor modification through smoking cessation, diet, exercise and medication like statins. For acute limb ischemia, initial treatment involves anticoagulation and endovascular procedures like thrombolysis or thrombectomy may be considered. Chronic PAD is managed through supervised exercise therapy and revascularization if needed.