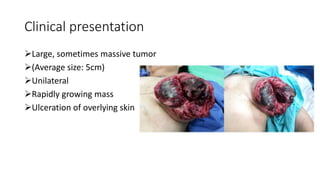
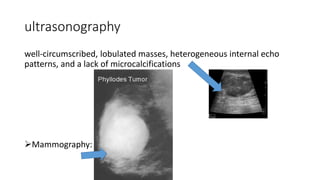
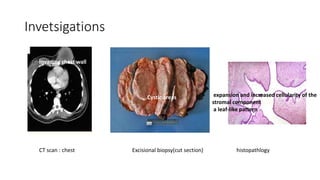
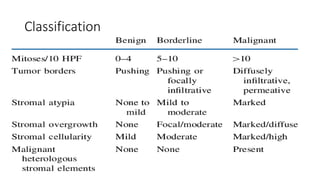
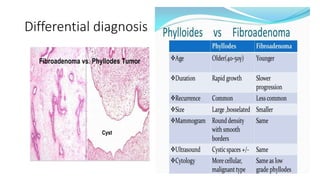
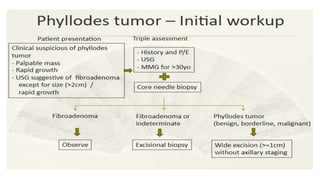
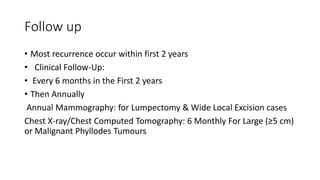
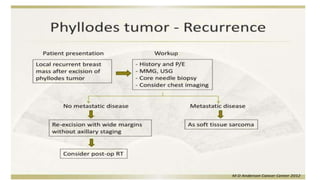
Phyllodes tumors are rare breast tumors that are usually benign but can sometimes be malignant. They make up 1% of breast tumors. Phyllodes tumors typically present as large, rapidly growing masses in women over 40 years old. Diagnosis is made through biopsy and imaging tests. Treatment is complete surgical excision with wide margins. For malignant tumors, adjuvant radiation or chemotherapy may be considered. Prognosis is generally good for benign and borderline tumors treated with surgery alone, while malignant tumors have a 5-year survival rate of 60-80% even with additional treatment.