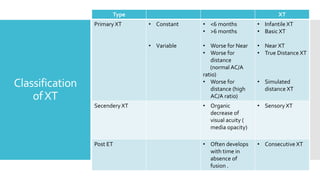
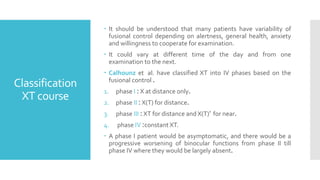
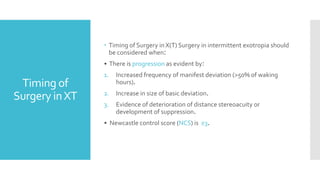
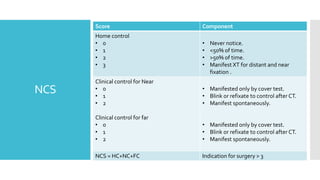
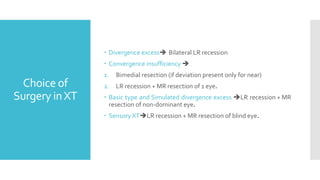
This document provides an overview of exotropia (XT), which is an outward deviation of one or both eyes. It classifies XT as primary, secondary, or post-ET. Primary XT can be constant, variable, infantile, or true/simulated distance. Symptoms include diplopia, asthenopia, or photophobia as exophoria decompensates. For management, full refractive correction is first followed by surgery if deviation is over 15Δ and binocular vision deteriorates. Surgery choices depend on type of XT such as bilateral lateral rectus recession for divergence excess or recession/resection for basic/simulated divergence excess XT. The document also discusses classification systems for X