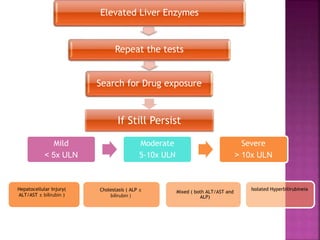
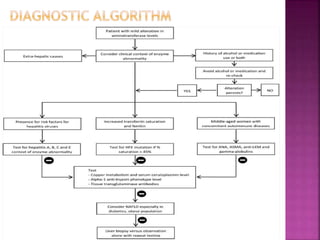
The document is a review article published in the Journal of Clinical and Translational Hepatology discussing the challenges of evaluating abnormal liver enzyme levels in asymptomatic patients. It emphasizes the importance of thorough history taking, clinical examinations, and laboratory investigations to identify potential causes while addressing relevant risk factors for liver disease. The article also covers diagnostic approaches for various conditions related to elevated liver enzymes, including chronic and acute liver diseases.