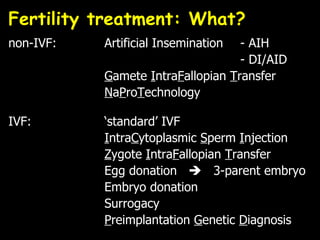
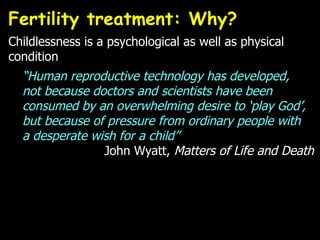
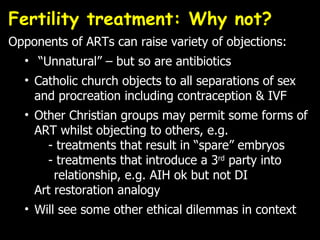
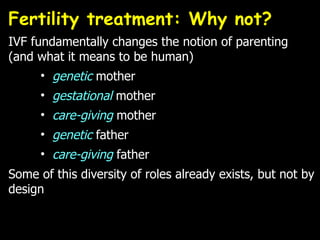
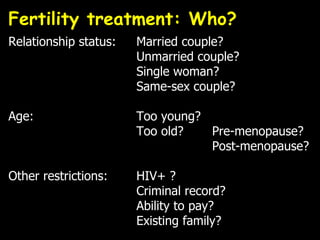
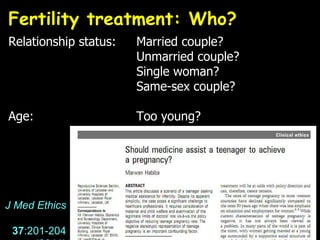
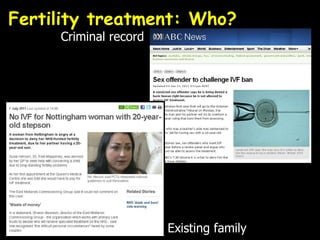
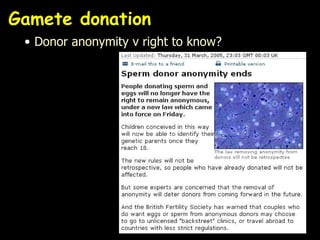
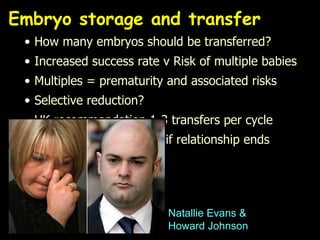
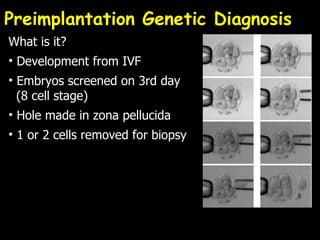
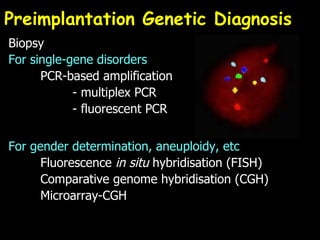
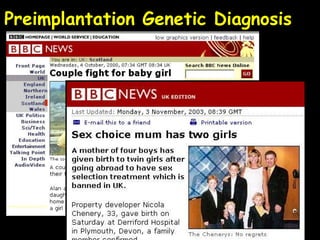
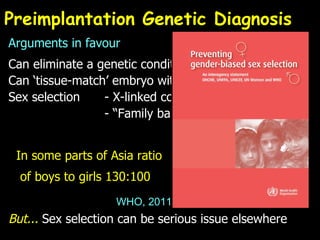
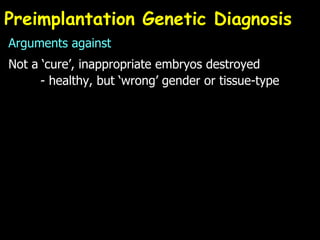
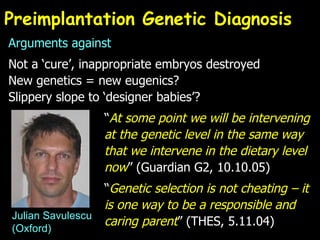
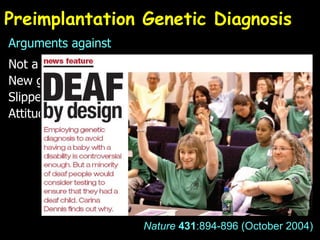
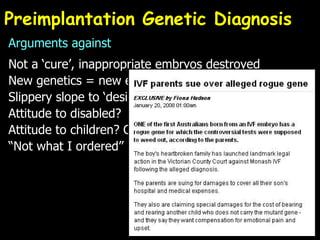
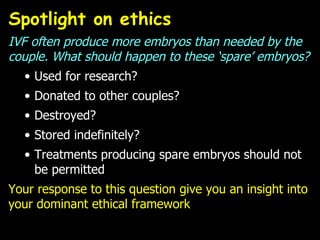
Dr. Chris Willmott gave a presentation on the ethical issues associated with fertility treatment. He discussed various fertility procedures like IVF, egg/embryo donation, and surrogacy. He also outlined some of the debates around who should have access to treatment, how many embryos should be transferred, the fate of leftover embryos, genetic screening of embryos, and resource allocation issues. The talk examined arguments both for and against different procedures from various ethical perspectives.
![Dr Chris Willmott Dept of Biochemistry, University of Leicester [email_address] Ethical issues associated with fertility treatment TSN Masterclass: “Reproductive Technologies” University of Leicester](https://image.slidesharecdn.com/ethicsoffertilitytreatments-110712154912-phpapp01/85/Ethical-issues-associated-with-fertility-treatment-1-320.jpg)


![Any Questions? E-mail : [email_address] Twitter : cjrw Slideshare : cjrw2 Delicious : chriswillmott Blogs : www.bioethicsbytes.wordpress.com www.biosciencecareers.wordpress.com www.lefthandedbiochemist.wordpress.com University of Leicester](https://image.slidesharecdn.com/ethicsoffertilitytreatments-110712154912-phpapp01/85/Ethical-issues-associated-with-fertility-treatment-36-320.jpg)