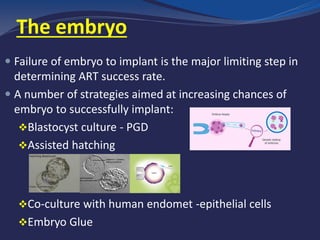
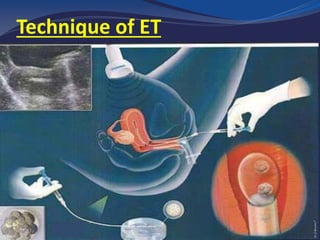
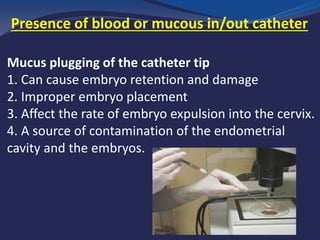
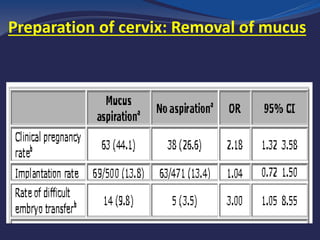
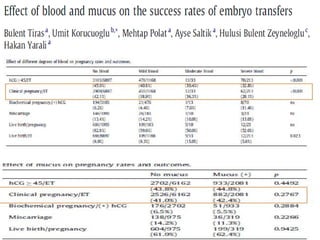
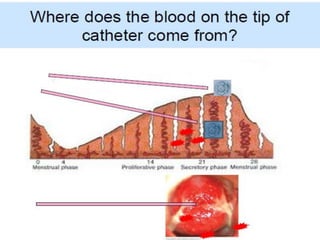
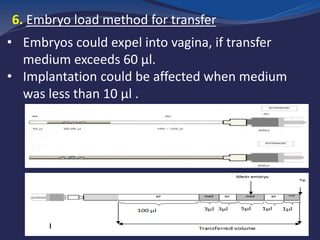
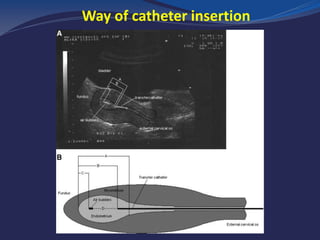
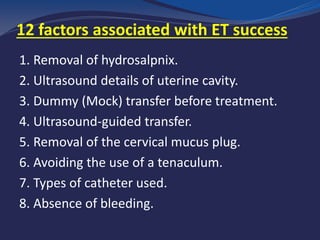
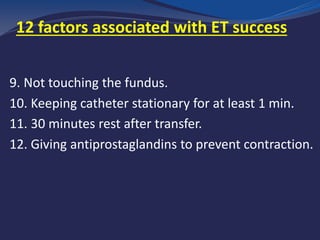
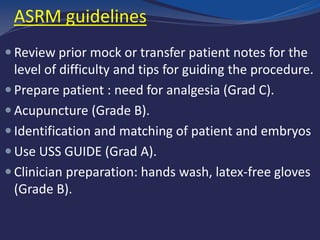
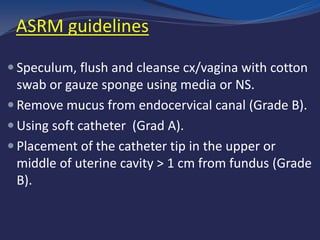
The embryo transfer technique is the final and most crucial step of the IVF cycle. It requires close collaboration between the clinician and embryologist. While around 80% of embryos typically reach the transfer stage, the pregnancy rate remains low due to factors such as poor embryo quality and technique. The success of embryo transfer depends on proper preparation, including evaluating the cervico-uterine axis, clearing mucus from the cervix, and using ultrasound guidance. The embryo must be placed in the optimal location of the uterine cavity to maximize implantation chances. Attention to factors such as catheter type, duration of embryo loading, and prevention of uterine contractions can significantly improve clinical pregnancy outcomes.