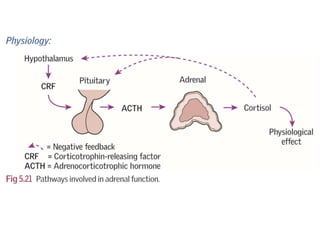
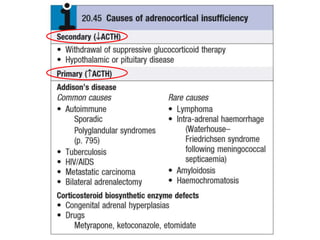
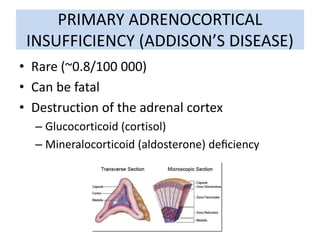
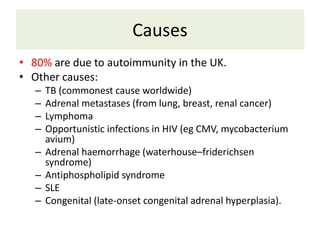
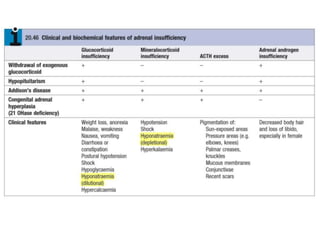
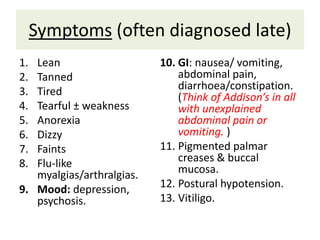
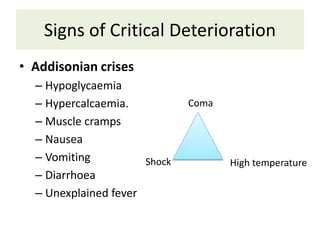
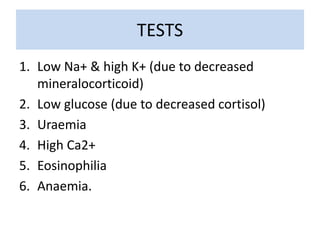
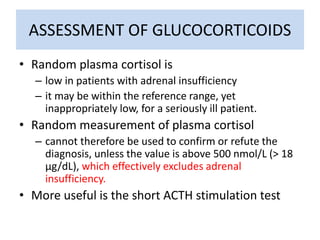
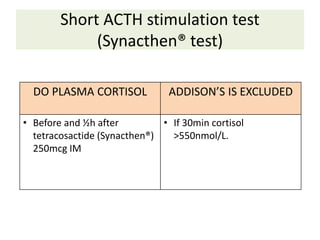
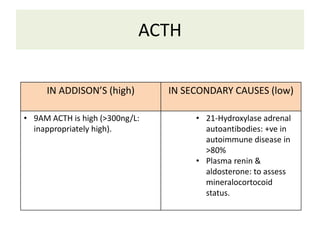
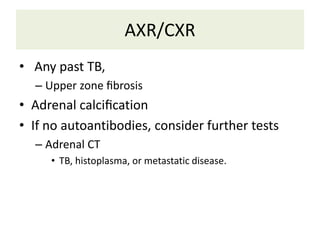
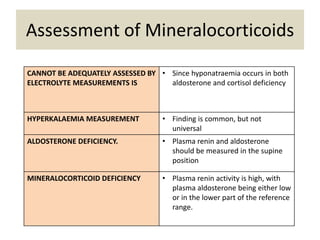
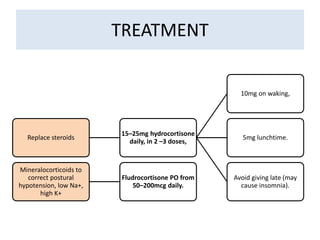
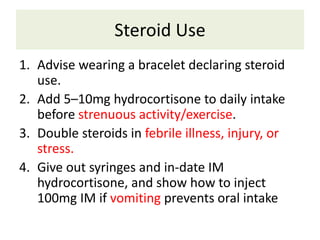
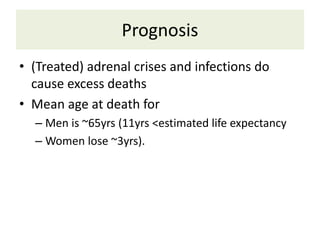
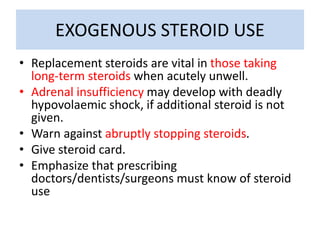
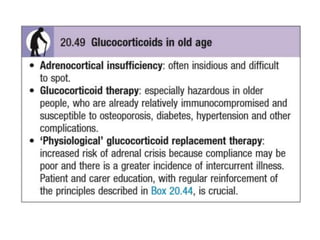
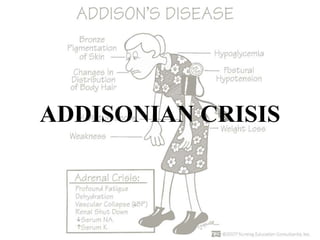
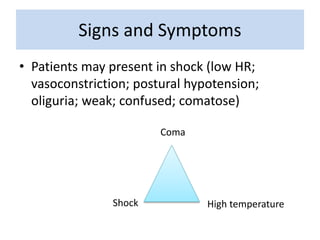
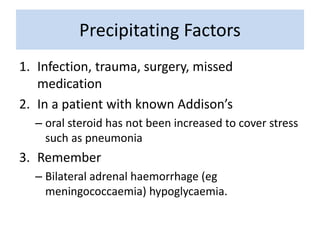
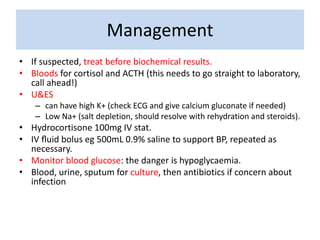
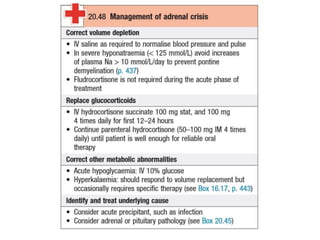
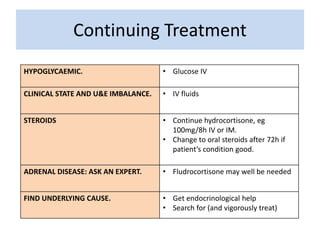
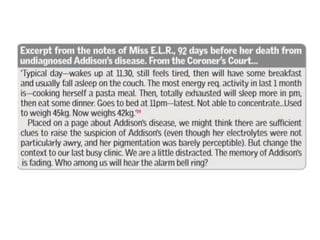
Adrenal insufficiency, also known as Addison's disease, is caused by destruction of the adrenal cortex leading to deficiencies in glucocorticoids and mineralocorticoids. It presents with non-specific symptoms like fatigue, weight loss, and low blood pressure. Diagnosis involves low cortisol levels in response to ACTH stimulation and high ACTH levels. Treatment is lifelong glucocorticoid and mineralocorticoid replacement. An adrenal crisis can result from infection or stress and requires immediate high dose glucocorticoid treatment in addition to intravenous fluids and glucose to prevent shock.