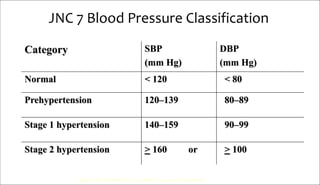
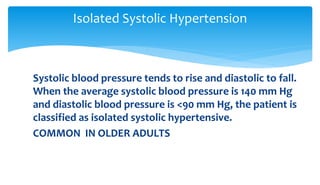
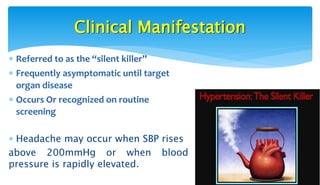
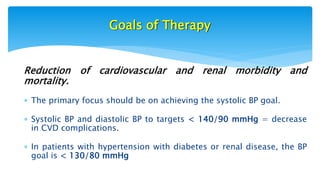
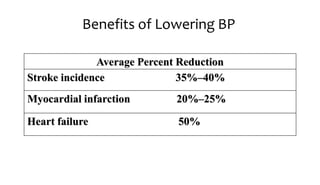
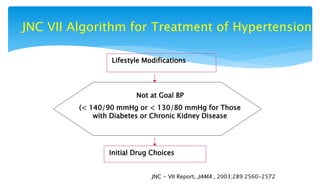
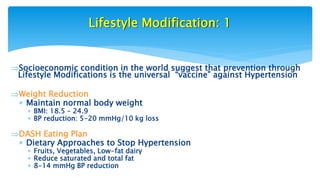
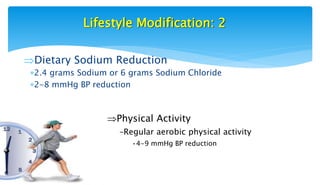
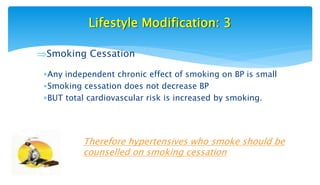
Hypertension, or high blood pressure, affects nearly 1 billion people worldwide. It is a leading cause of death and is poorly controlled in many countries. May 14th is recognized as World Hypertension Day to increase awareness. Hypertension is defined as a systolic blood pressure over 140 mmHg or a diastolic over 90 mmHg. Lifestyle modifications like weight loss, dietary changes, and increased physical activity can help control blood pressure but medication is often required. Treatment goals are to reduce blood pressure below 140/90 mmHg or 130/80 for those with diabetes or kidney disease to lower the risks of complications.

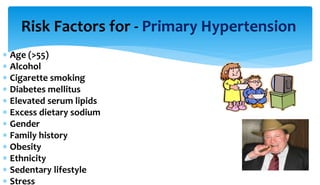
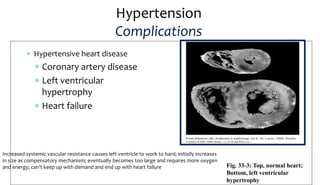
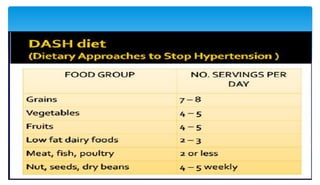
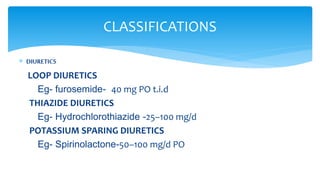
![Factors Influencing
Blood Pressure (BP)
Cardiac output is total blood flow through systemic or pulmonary
circulation per min. CO =stroke volume (amt pumped out of
L ventricle per beat [70 ml]) times the HR for 1 min.
SVR + force opposing movement of blood in vessels;
determined primarily by radius of small arteries & arterioles
Blood
Pressure
Cardiac
Output
Systemic
Vascular
Resistance
= x
Copyright © 2007, 2004, 2000, Mosby, Inc., an affiliate of Elsevier Inc. All Rights Reserved.](https://image.slidesharecdn.com/hypertension-170817105635/85/Hypertension-4-320.jpg)
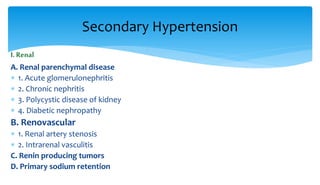
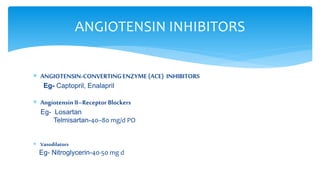
![ Hypertension is a persistent systolic blood pressure
greater than 140 mm Hg and a diastolic pressure greater
than 90 mm Hg or current use of antihypertensive
medication
(Seventh Report of the Joint National Committee on Prevention,
Detection, Evaluation, and Treatment of High Blood Pressure [JNC
VI]
DEFINITION](https://image.slidesharecdn.com/hypertension-170817105635/85/Hypertension-9-320.jpg)