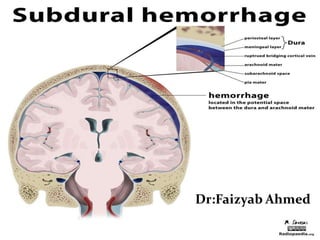
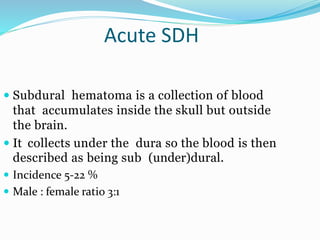
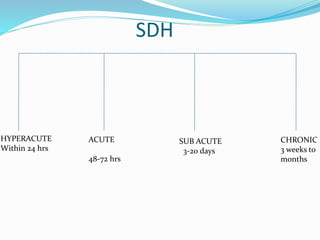
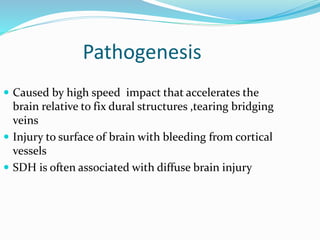
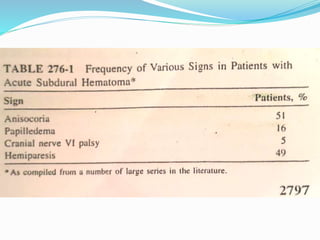
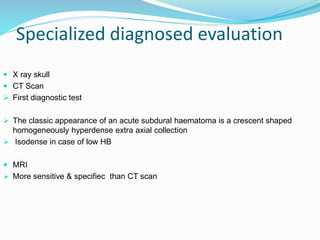
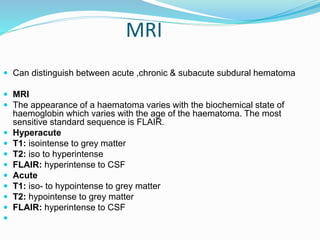
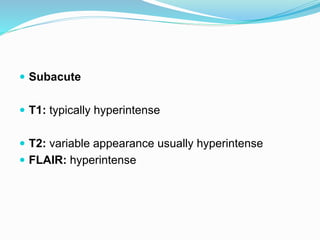
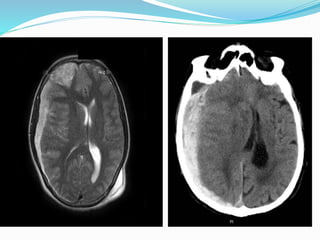
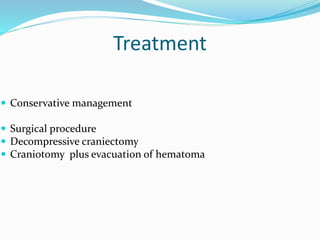
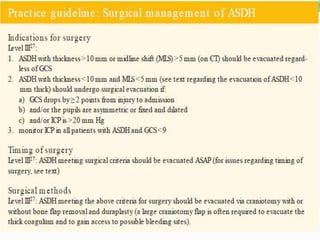
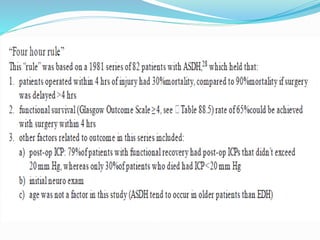
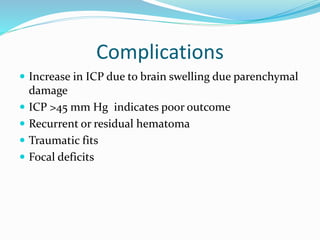
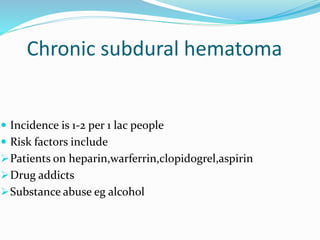
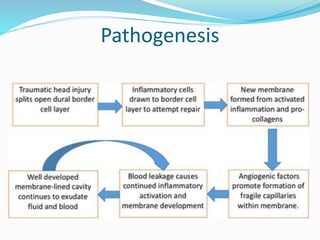
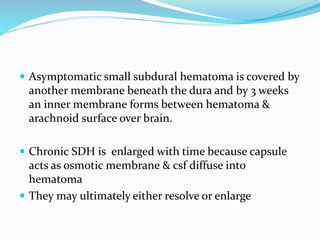
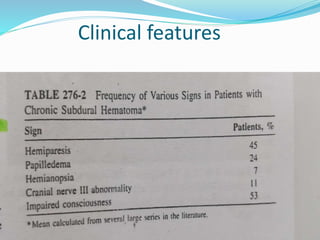
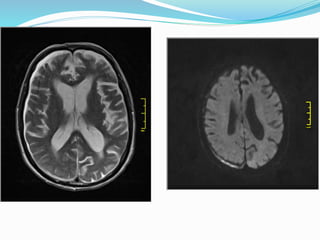
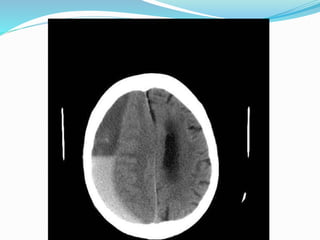
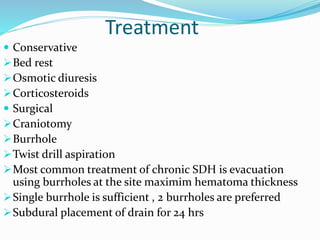
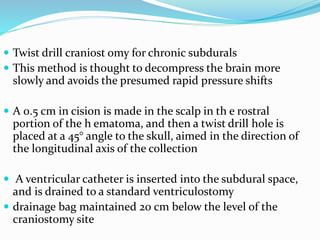
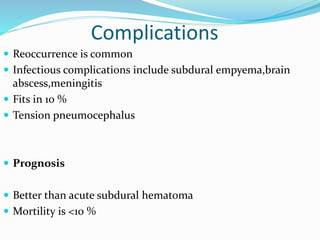
Subdural hematoma (SDH) is a blood accumulation between the skull and brain caused by high-speed impact, with varying incidence and gender ratios. Diagnosis typically involves CT or MRI scans to determine the type and stage of the hematoma, while treatment options include conservative management and surgical interventions. Complications may include increased intracranial pressure and recurrence, with prognosis varying based on the type of SDH and initial clinical state.