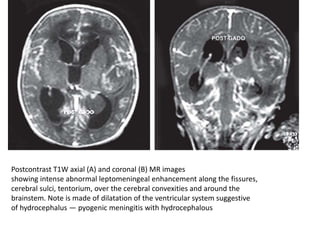
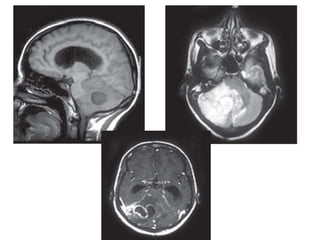
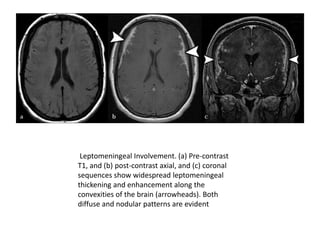
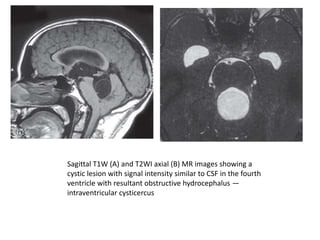
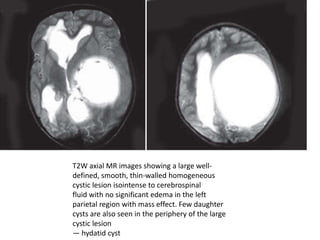
This document summarizes various central nervous system infections, including bacterial/pyogenic meningitis, tuberculous meningitis, and intracranial tuberculomas. Key imaging findings are described, such as meningeal enhancement on CT/MRI for meningitis and ring enhancement on CT/MRI for brain abscesses. Complications like hydrocephalus, infarctions, and ventriculitis are also discussed. MR spectroscopy findings that can help differentiate tuberculomas from other lesions are mentioned.