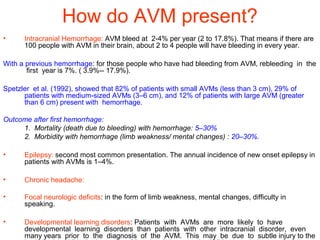
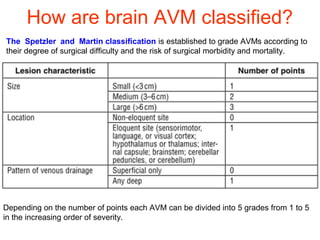
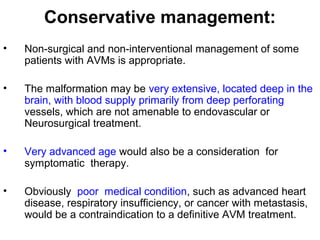
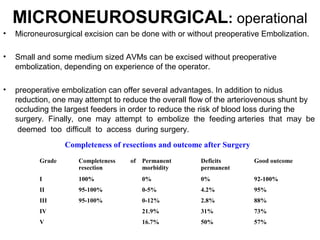
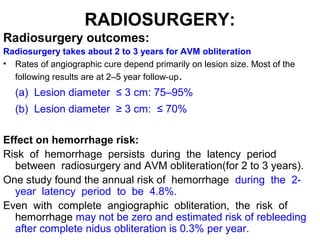
Brain arteriovenous malformations (AVMs) are abnormal clusters of blood vessels in the brain. They can cause bleeding in the brain or seizures. AVMs are typically treated through surgery to remove the abnormal vessels, procedures to block the blood vessels using embolization, or radiation therapy to damage the vessels. Each treatment has risks of complications like bleeding in the brain, infections, or neurological deficits. The best treatment depends on the size and location of the AVM. Conservative management without intervention may be appropriate for some patients as well.