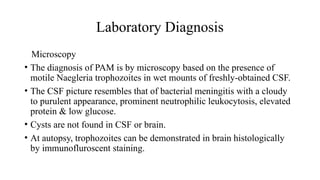
Amoebae are membrane-bound protozoan parasites that can be free-living or parasitic, with Entamoeba histolytica being a notable pathogenic species associated with intestinal amoebiasis. The document outlines the life cycle, clinical presentation, epidemiology, and treatment of amoebiasis, highlighting the prevalence in areas with poor sanitation and the potential for asymptomatic carriers to spread the infection. Additionally, it discusses free-living amoebae such as Naegleria fowleri and Acanthamoeba, known to cause severe infections like primary amoebic meningoencephalitis.