1) Acute gastrointestinal bleeding can originate from the upper GI tract and has many potential causes, including peptic ulcers, esophageal and gastric varices, erosive mucosal disease, and tumors.
2) Initial management involves resuscitation, localization of the bleeding site, and initiation of pharmacotherapy or endoscopic therapy to stop active bleeding.
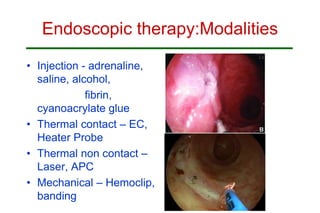
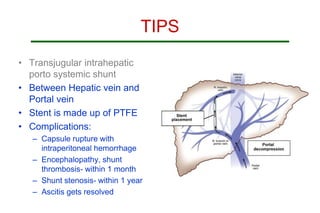
3) Specific treatments depend on the underlying cause, with peptic ulcers commonly treated with proton pump inhibitors, endoscopic therapy, and surgery if bleeding persists, while variceal bleeding is managed with vasoactive drugs, balloon tamponade, endoscopic band ligation or sclerotherapy, and TIPS procedure.