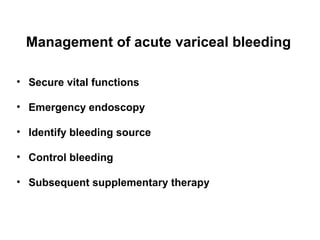
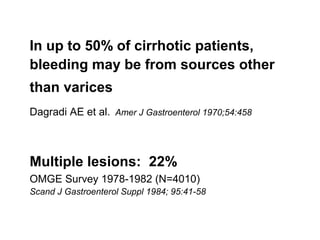
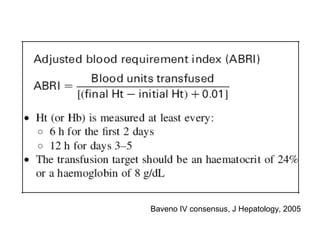
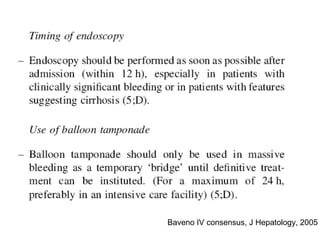
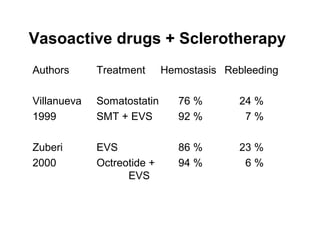
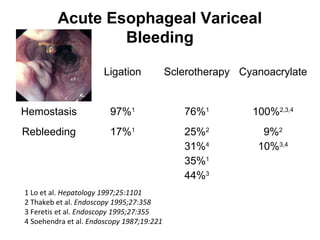
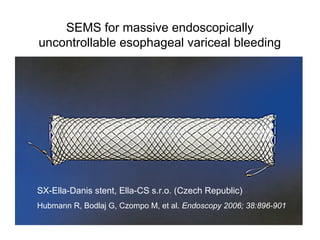
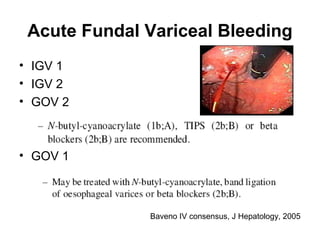
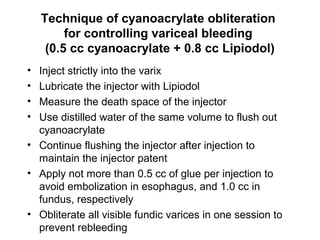
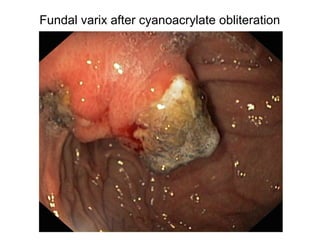
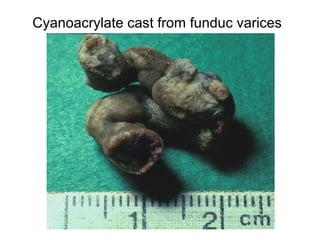
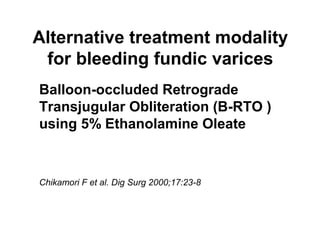
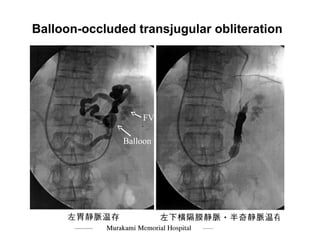
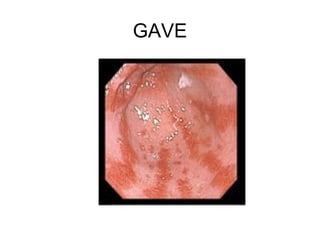
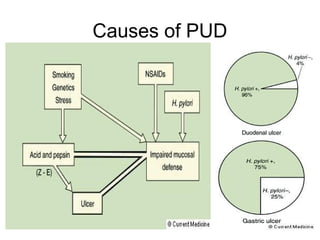
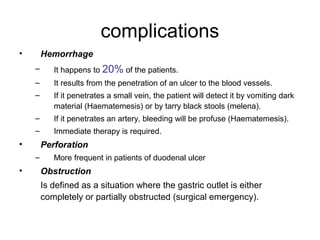
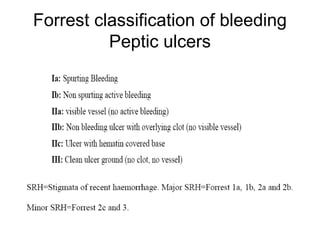
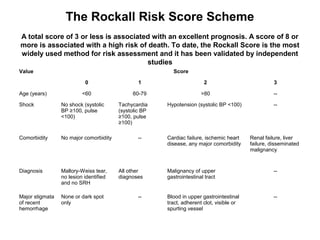
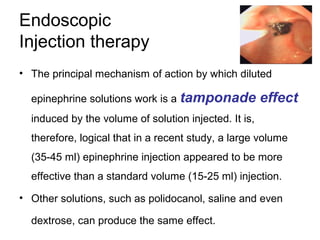
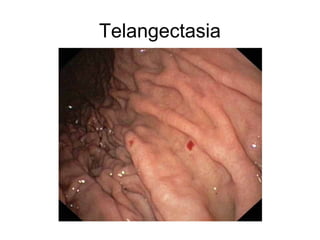
This document discusses the causes and management of upper gastrointestinal bleeding. It begins by listing common causes such as portal hypertension, peptic ulcer disease, angiomatous malformations, and neoplasms. For portal hypertension, it focuses on variceal bleeding and techniques for controlling acute variceal hemorrhage such as band ligation, sclerotherapy, and cyanoacrylate injection. For peptic ulcer disease, it covers risk assessment using the Forrest classification and Rockall score, medical and endoscopic treatment options, and the role of H. pylori eradication. It also briefly discusses less common causes of upper GI bleeding like Dieulafoy lesions and telangectasia.