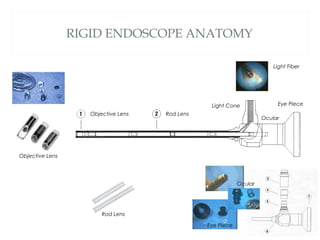
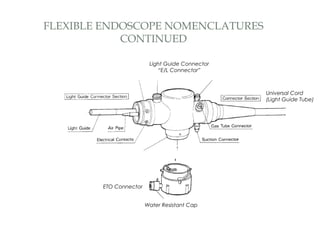
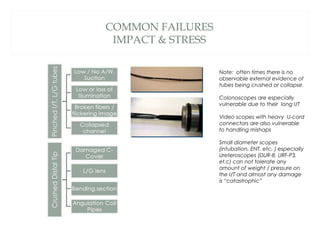
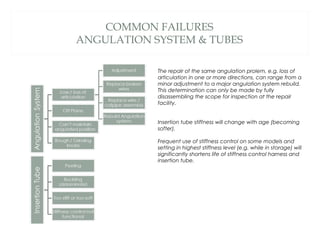
The document provides an inservice introduction to endoscopes, highlighting that 70% of repairs result from accidents and emphasizing the importance of education and training in accident prevention. It details the functionalities, specifications, common failures, and best practices for managing repair expenditures of endoscopes. The presentation aims to enhance awareness of proper care for these delicate devices and offers resources for further learning and assistance.