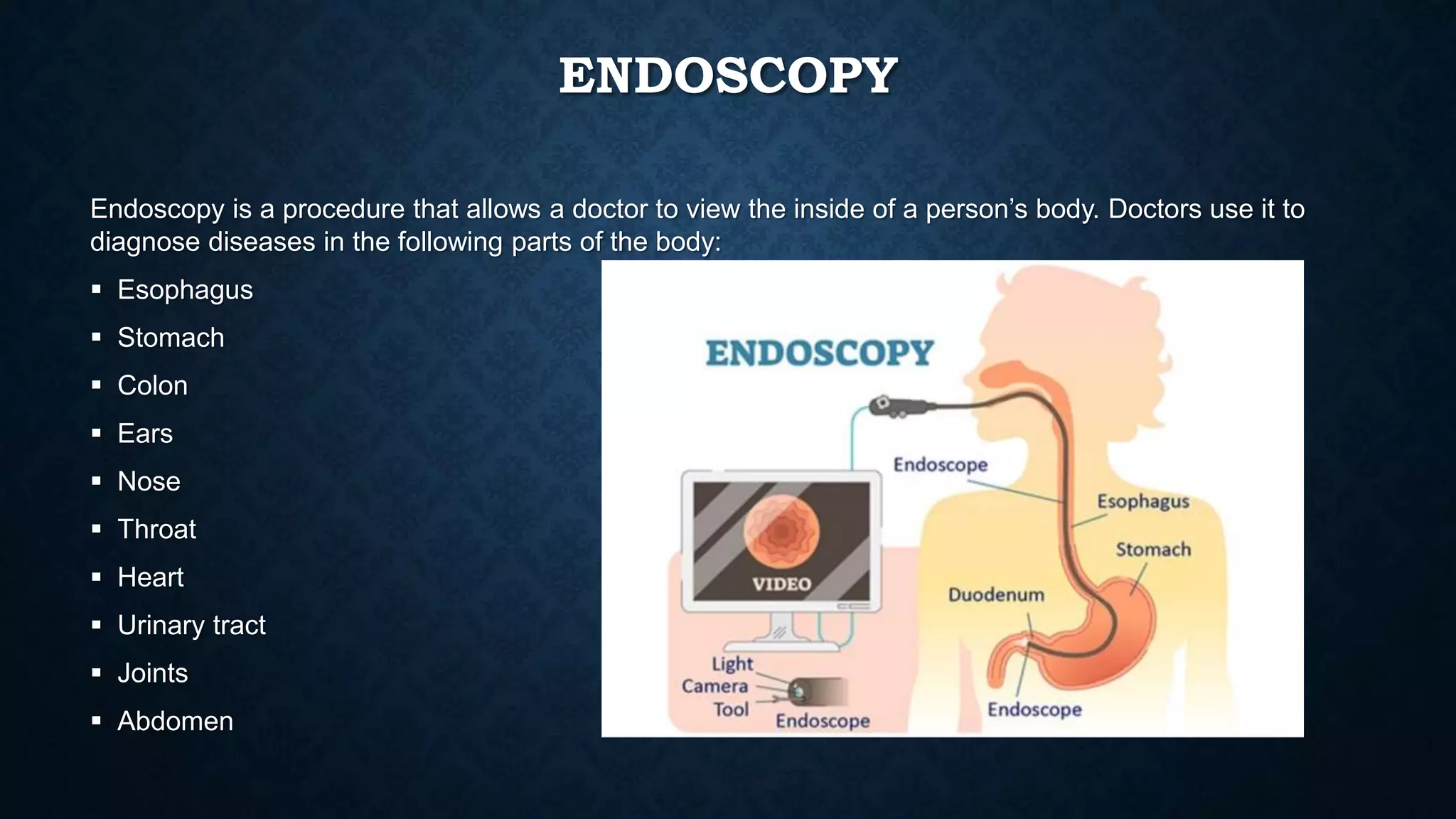
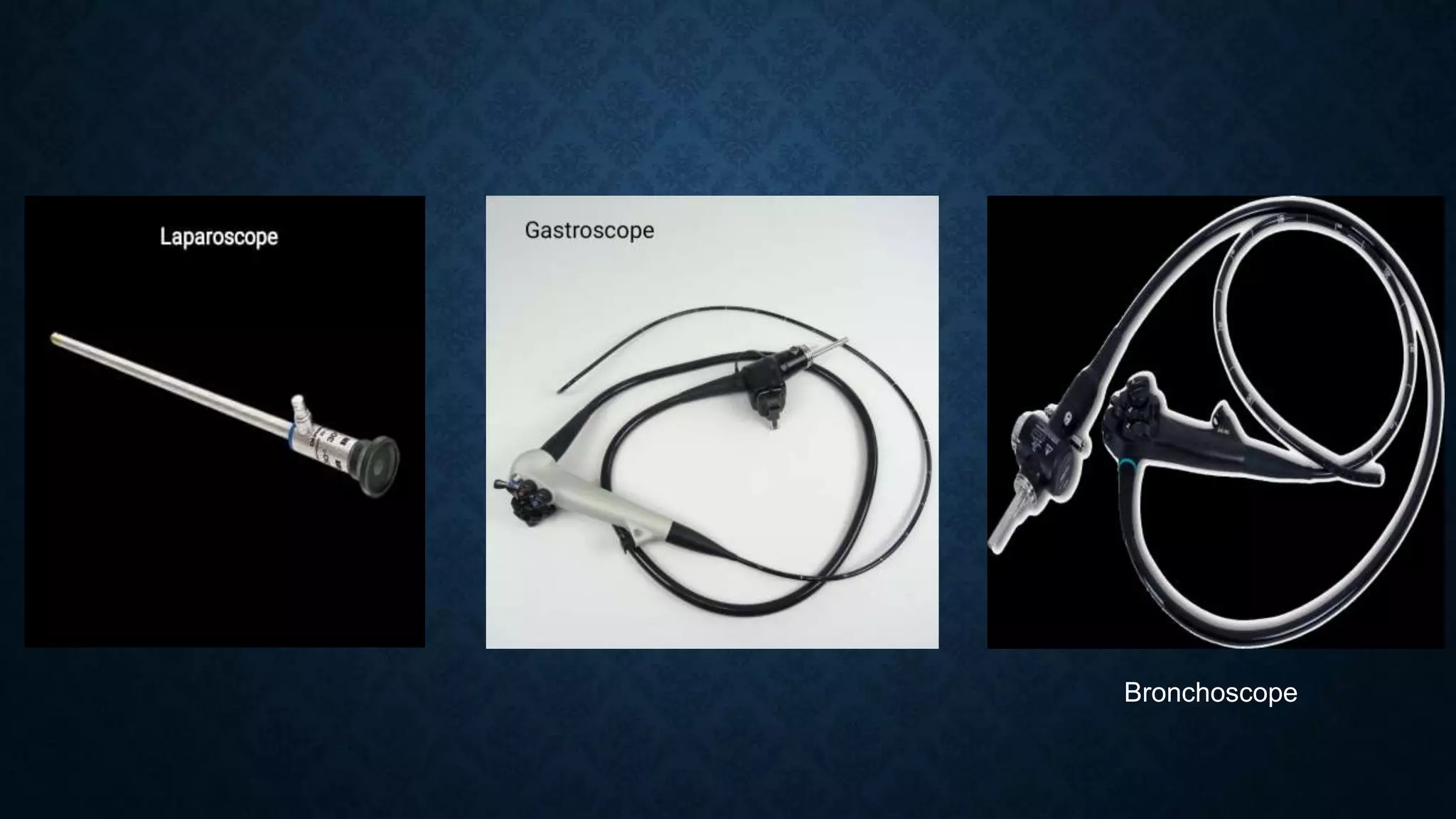
An endoscope is a thin, flexible tube used in endoscopy procedures to examine the inside of the body. It has a light and camera at the end to provide visuals. Endoscopes come in different shapes depending on the part of the body being examined. They are used to diagnose diseases in organs like the esophagus, stomach, and colon. Endoscopy allows doctors to view areas that cannot otherwise be seen. Proper cleaning, disinfection and storage of endoscopes is important for patient safety.