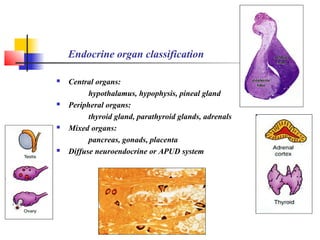
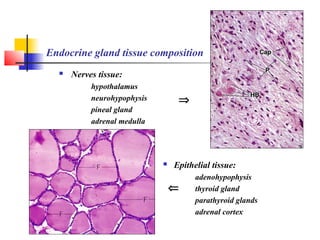
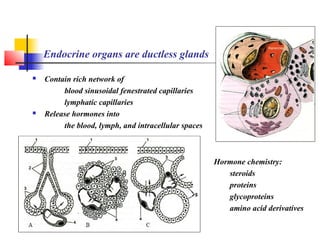
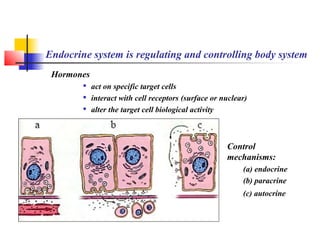
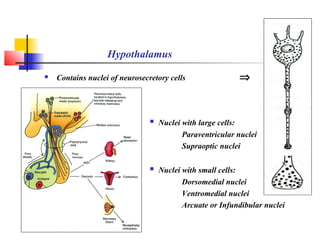
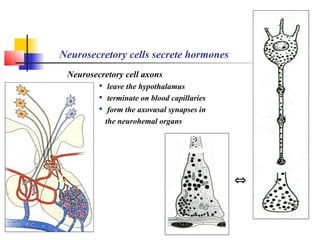
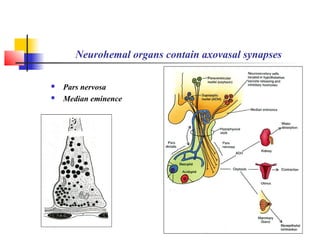
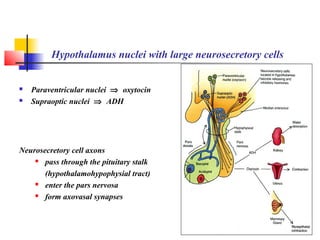
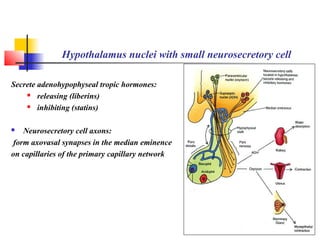
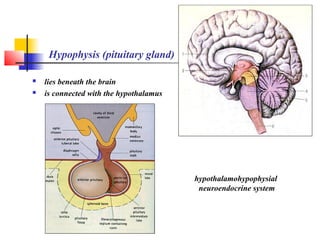
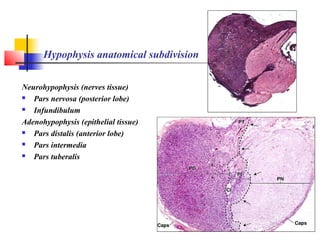
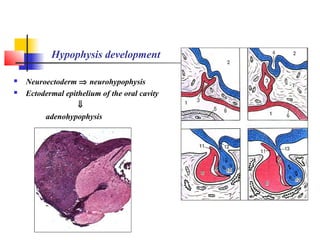
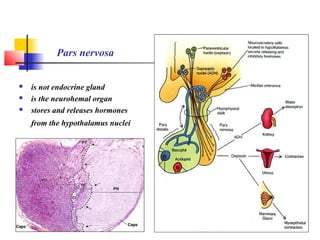
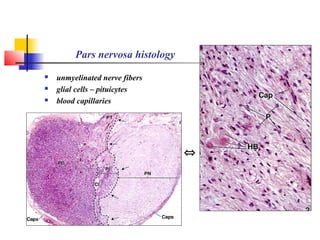
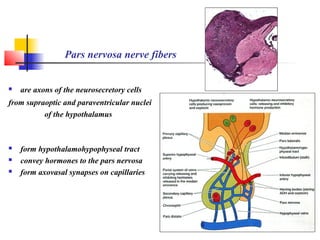
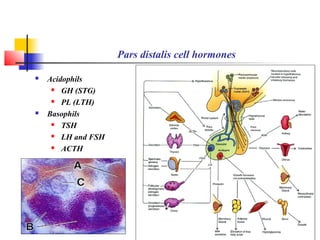
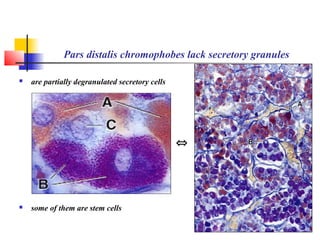
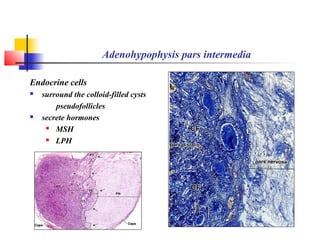
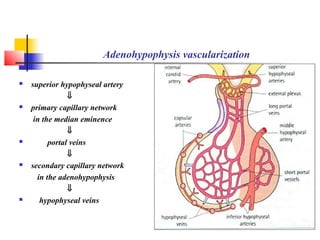
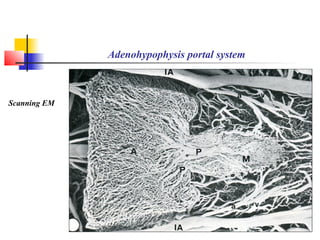
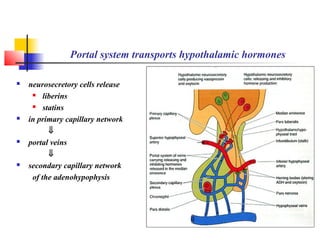
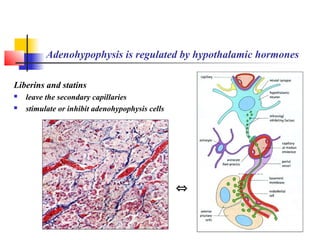
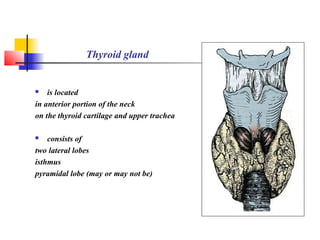
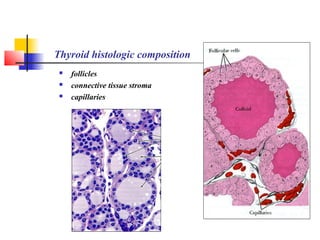
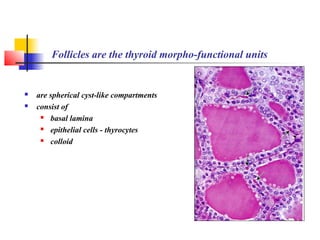
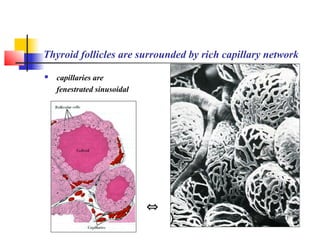
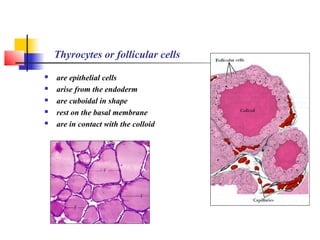
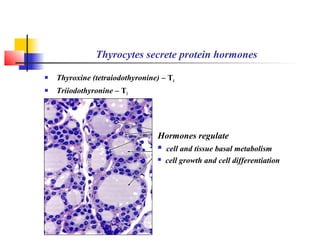
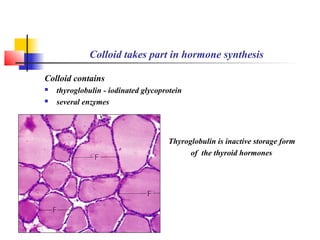
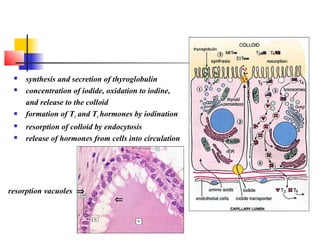
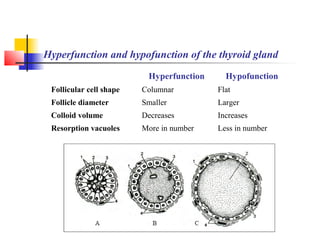
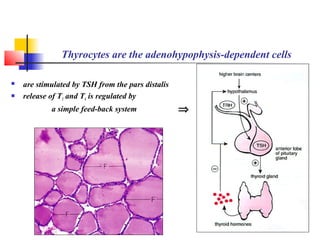
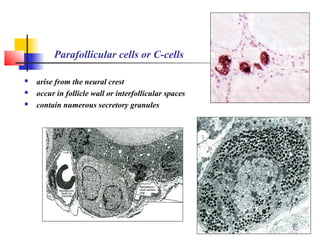
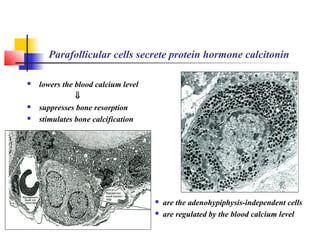
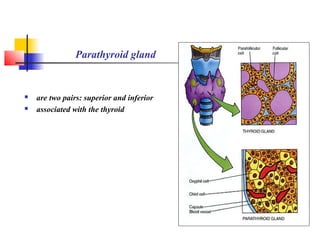
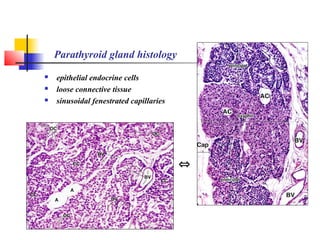
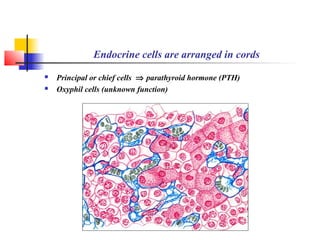
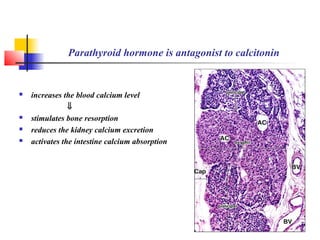
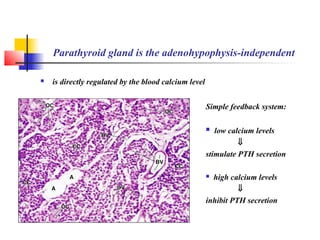
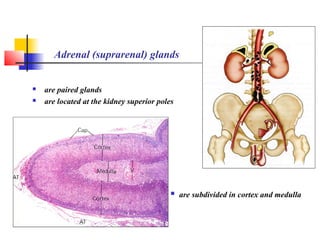
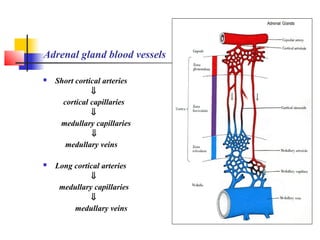
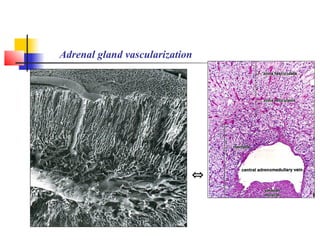
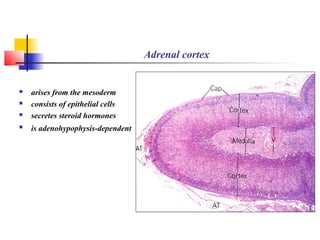
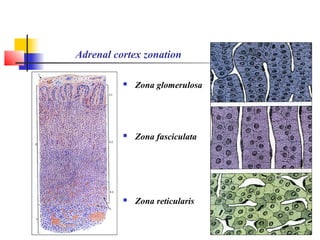
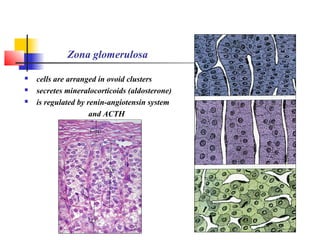
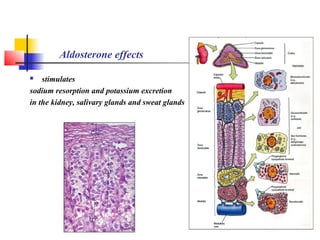
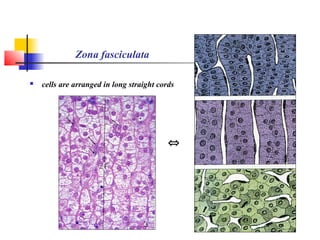
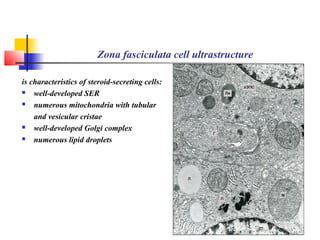
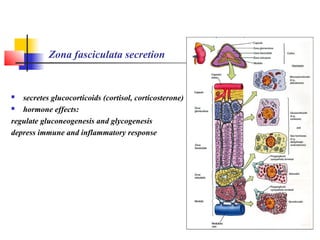
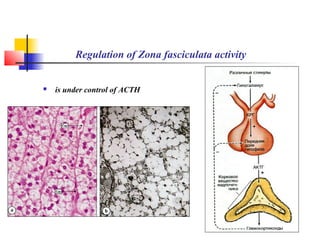
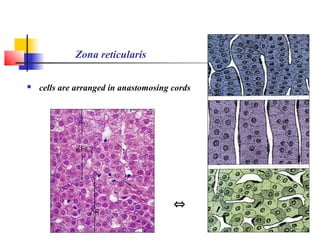
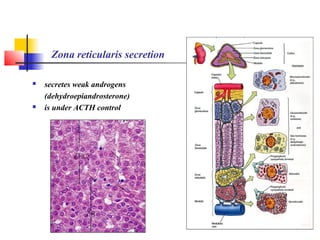
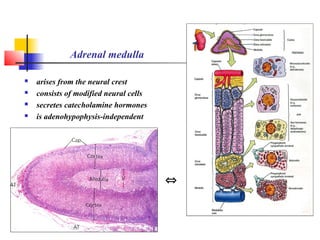
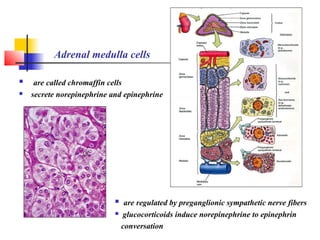
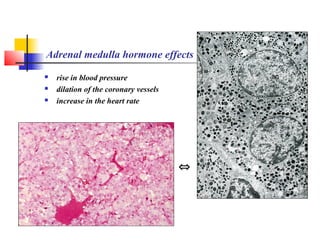
This document summarizes the major endocrine organs and their functions. It describes the classification of endocrine organs into central, peripheral, mixed and diffuse systems. It then details the key tissues and cells involved in hormone production for each organ, including the hypothalamus, hypophysis, thyroid gland, parathyroid glands, adrenal glands and pancreas. For each organ, it explains the histology, hormone production and regulation via feedback loops with other endocrine organs like the hypothalamus and hypophysis.