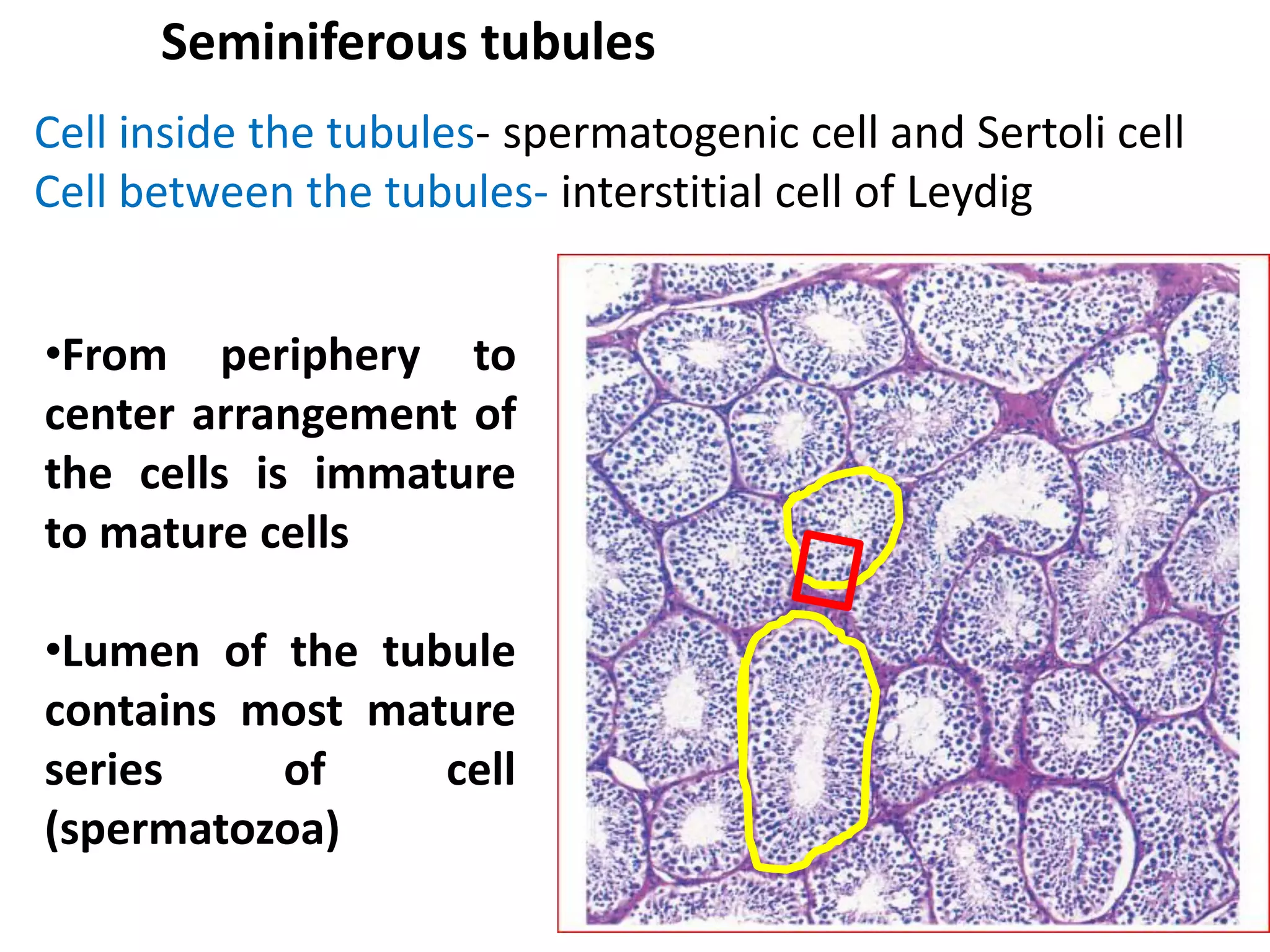
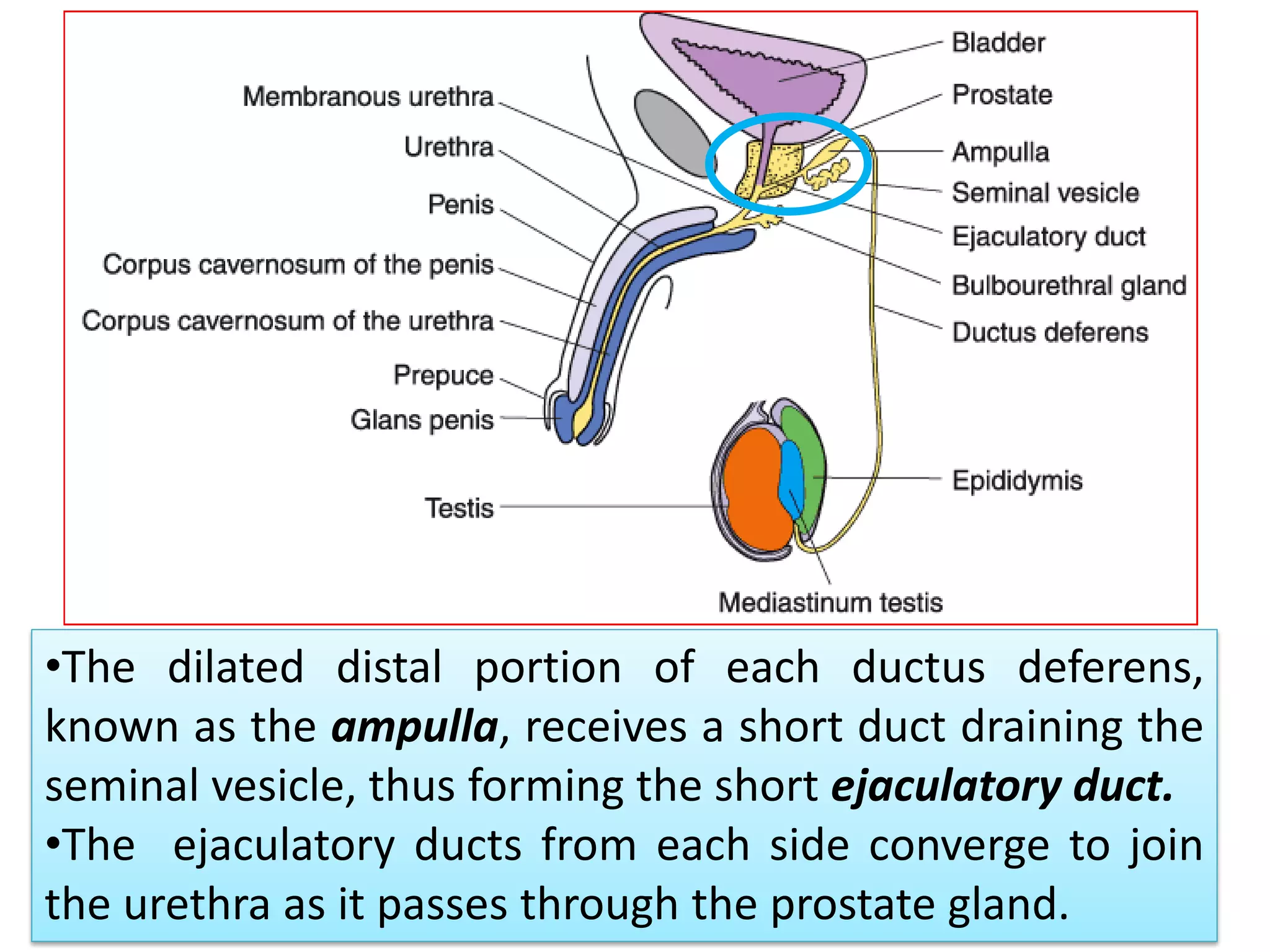
The document provides a comprehensive overview of the histology and anatomy of the male reproductive system, detailing the various components such as testis, epididymis, vas deferens, accessory glands, and penis. It highlights the functions of different cell types, including Leydig and Sertoli cells, and discusses conditions such as androgen insensitivity syndrome. The histological features of structures like the prostate gland, seminal vesicles, and the overall development and physiological processes involved in male reproduction are also summarized.