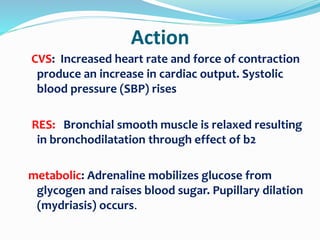
Positive inotropic drugs like adrenaline and noradrenaline increase myocardial contractility and cardiac output. Adrenaline acts on beta-1, beta-2, and alpha-1 receptors to increase heart rate, contractility, and blood pressure. It is used in low cardiac output states, shock, and bronchodilation. Noradrenaline is a potent vasoconstrictor that raises blood pressure through alpha-1 receptor activation with less tachycardia than adrenaline. Both drugs require close hemodynamic and ECG monitoring due to risks of hypertension, arrhythmias, and other side effects.