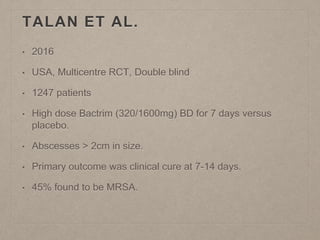
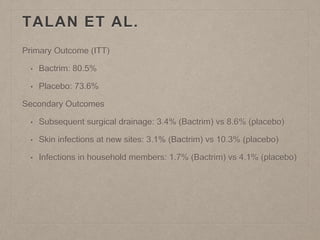
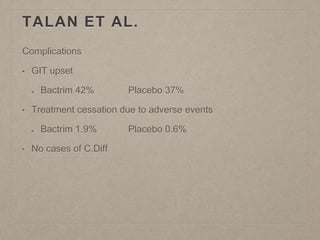
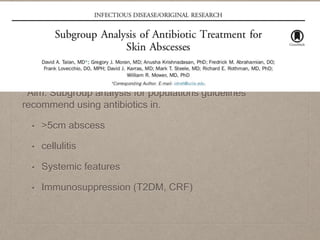
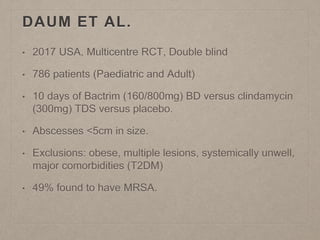
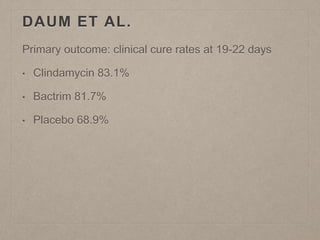
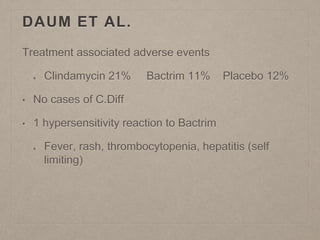
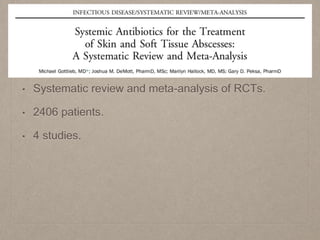
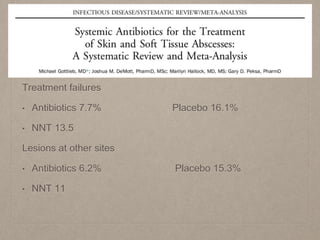
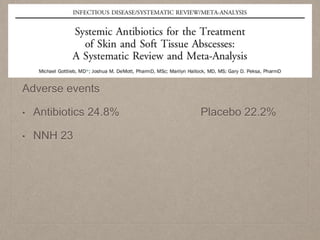
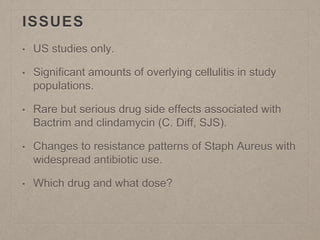
This document summarizes several studies on the use of antibiotics for abscess management. A 2016 RCT of over 1000 patients found that high-dose Bactrim led to higher cure rates of abscesses over 2cm compared to placebo, especially for those with MRSA, fevers, or immunosuppression. A 2017 RCT of under 800 patients found Bactrim and clindamycin had similar cure rates of abscesses under 5cm as placebo. However, antibiotics were associated with higher adverse gastrointestinal events. Overall, meta-analyses show antibiotics reduce treatment failures and new skin infections compared to incision and drainage alone, but with a risk of serious drug side effects.