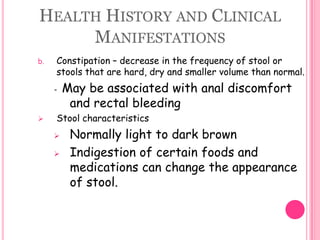
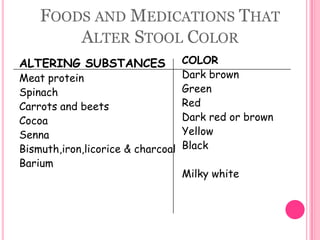
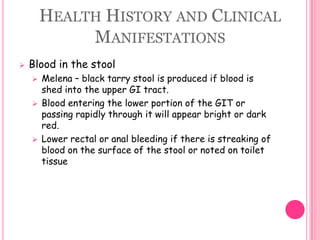
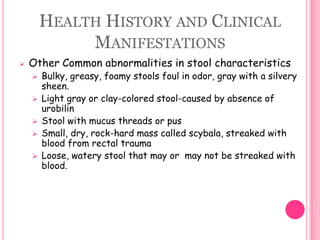
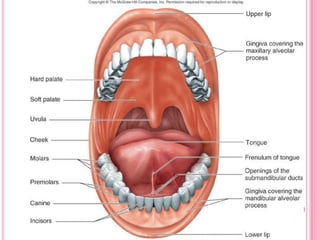
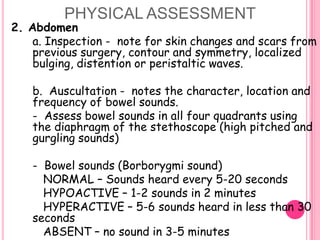
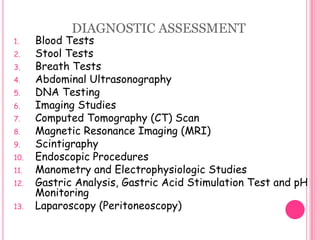
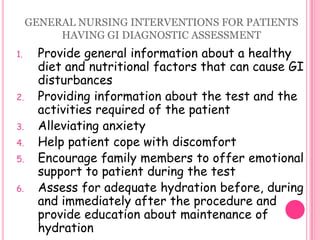
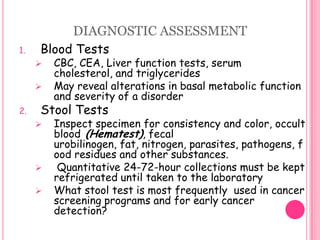
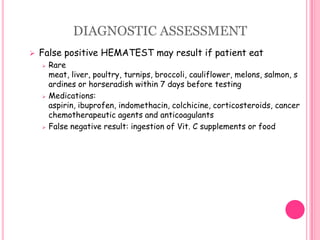
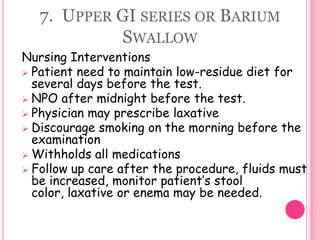
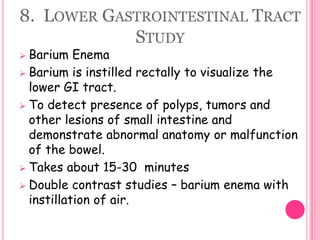
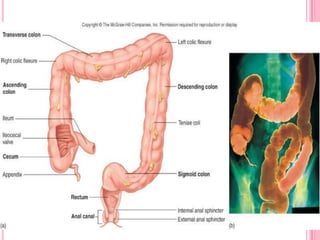
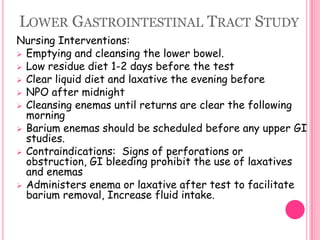
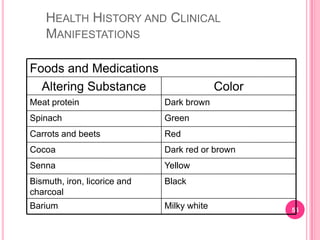
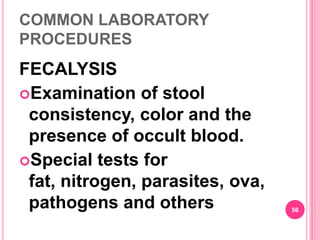
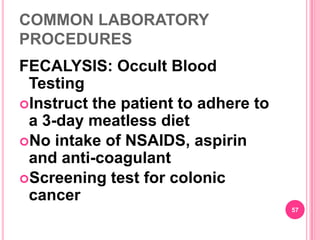
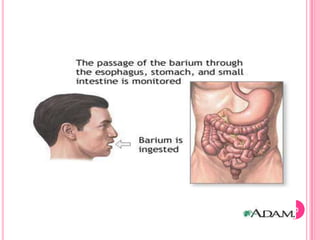
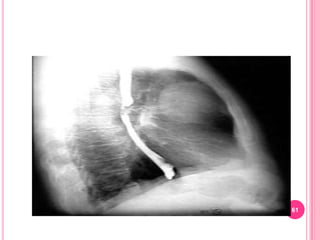
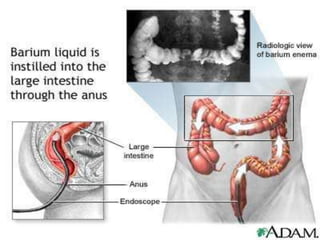
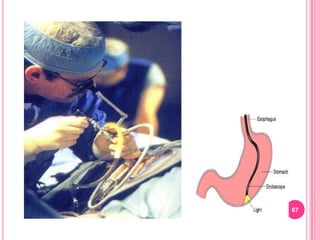
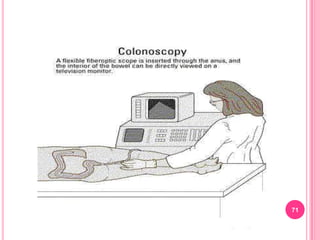
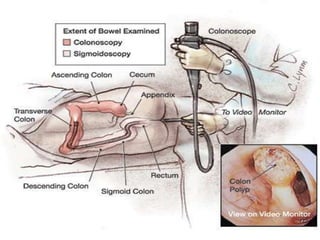
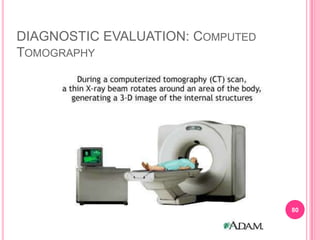
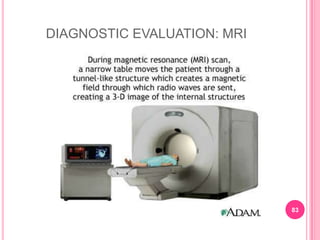
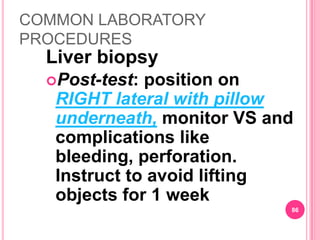
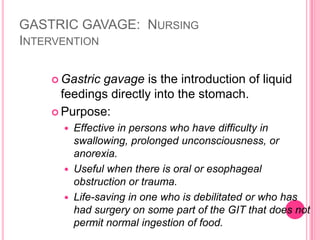
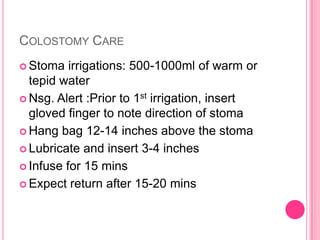
This document provides information on assessing patients for gastrointestinal issues. It outlines steps for a physical exam including inspection of the mouth and abdomen. It describes common GI symptoms like pain, indigestion, changes in bowel habits, and blood in the stool. Diagnostic tests are discussed including blood tests, stool tests, imaging studies, and endoscopy. Nursing interventions are described for preparing patients and providing care and education during diagnostic procedures.