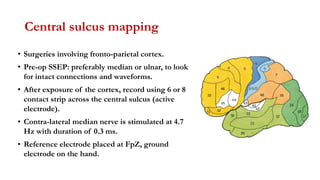
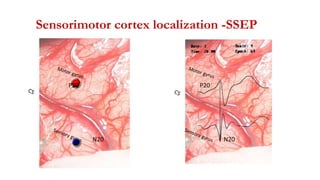
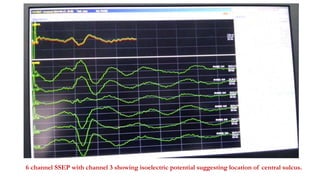
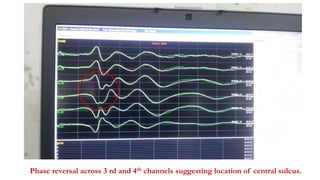
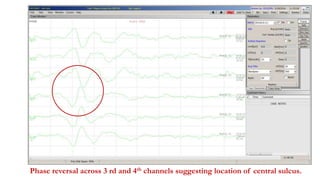
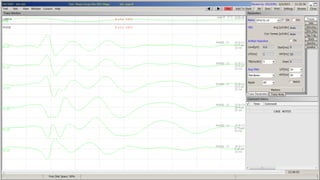
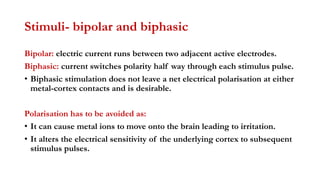
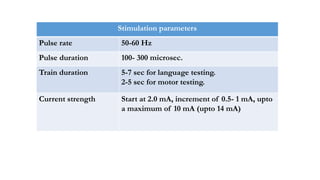
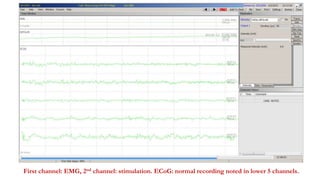
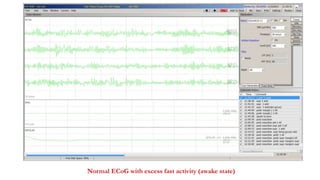
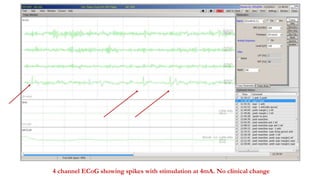
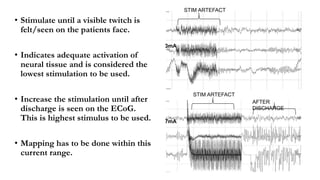
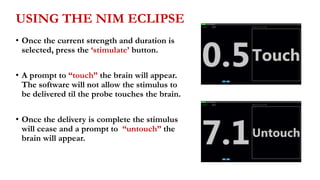
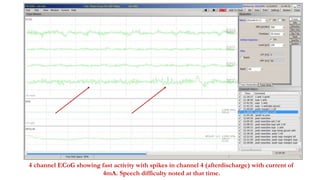
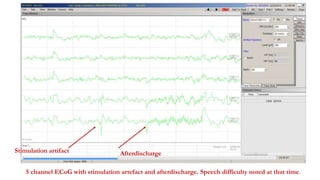
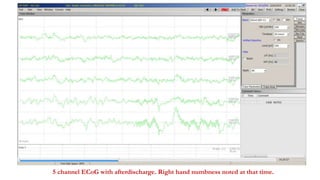
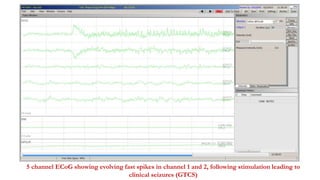
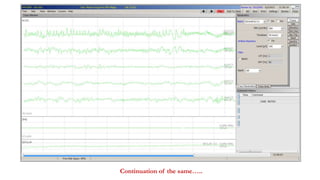
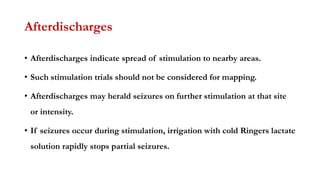
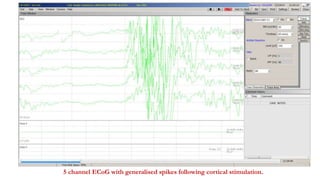
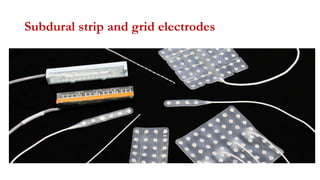
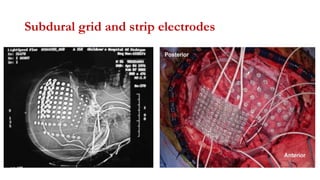
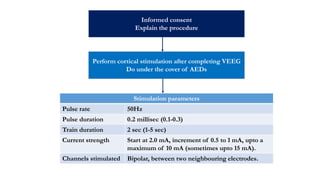
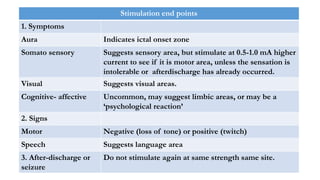
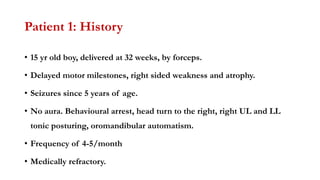
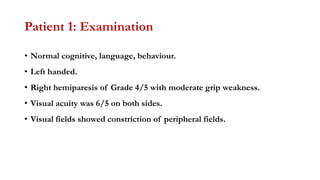
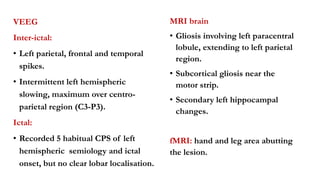
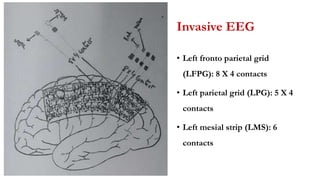
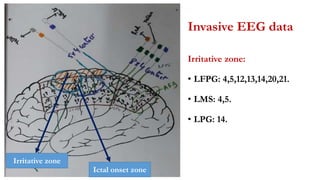
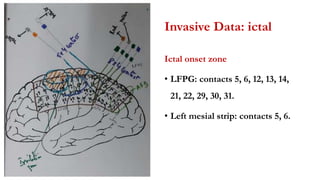
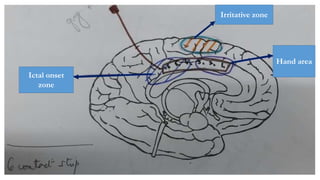
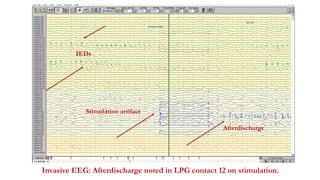
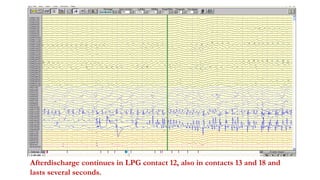
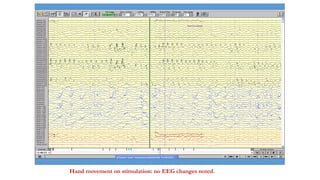
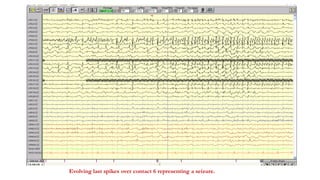
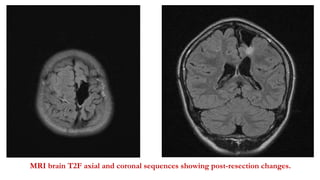
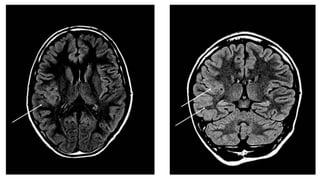
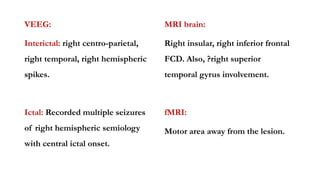
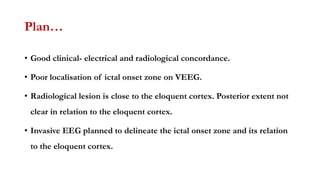
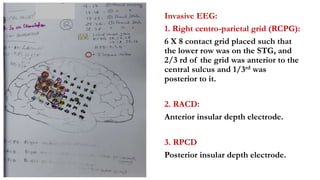
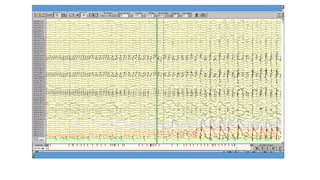
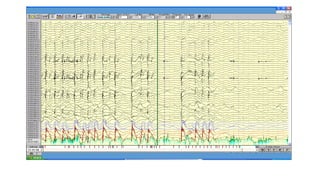
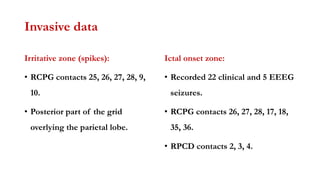
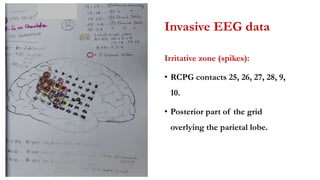
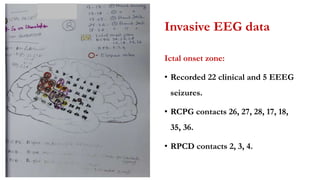
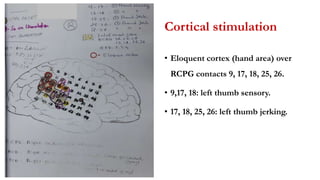
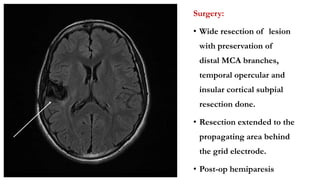
Cortical stimulation and mapping is used to localize functional areas of the brain before epilepsy surgery. There are two main methods - intraoperative using probes during surgery, and extraoperative using grids or strips placed on the brain surface. Central sulcus mapping uses stimulation of the median nerve and recording across the central sulcus to identify the motor cortex. Cortical stimulation parameters include bipolar pulses at 50-60Hz for language and motor mapping to elicit responses without afterdischarges. Two patient case studies demonstrate invasive EEG using grids and strips to further define the ictal onset zone and guide resection in relation to eloquent areas.