- A 55-year-old male presented with 3 weeks of weakness, fatigue, and weight loss. Physical exam found him to be thin and lean with oral pigmentation.
- Labs found leukopenia, a positive PPD test, low cortisol, increased ACTH, and a normal chest x-ray.
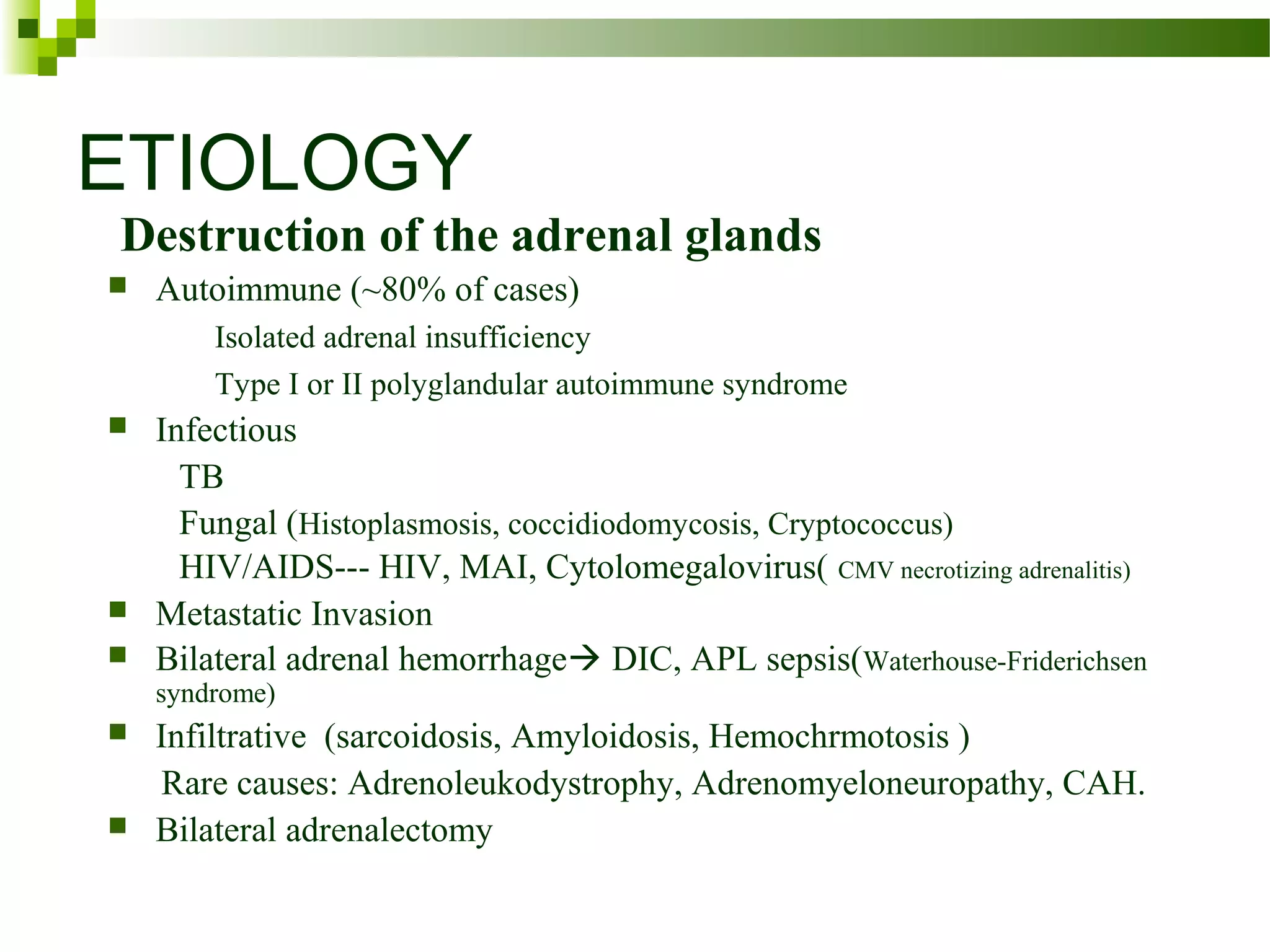
- The final diagnosis was tuberculosis adrenalitis, which had caused primary adrenal insufficiency.