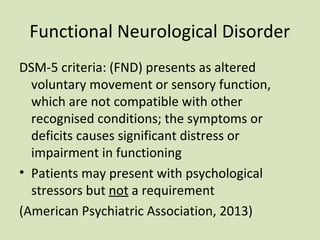
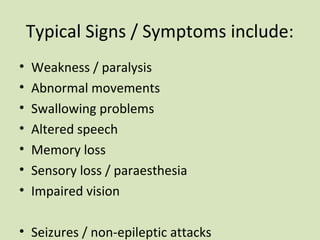
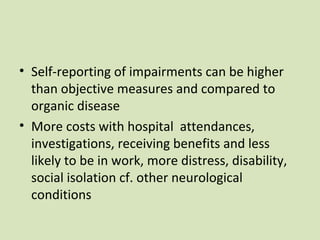
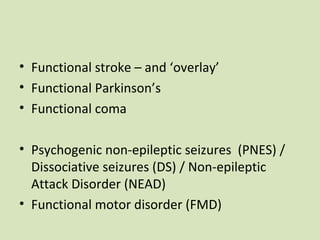
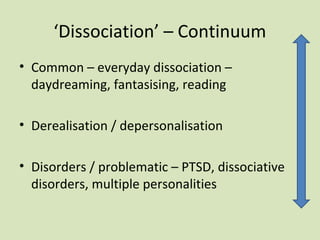
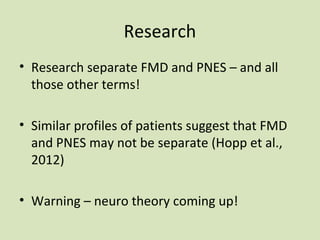
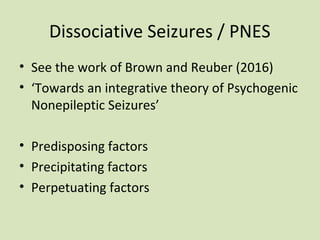
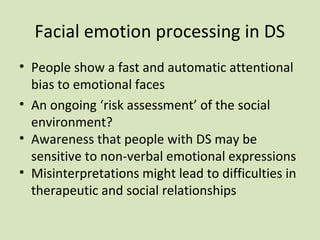
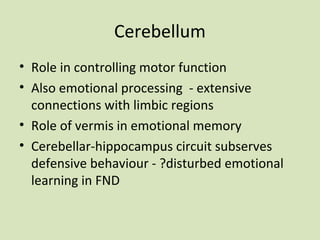
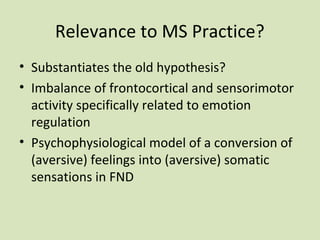
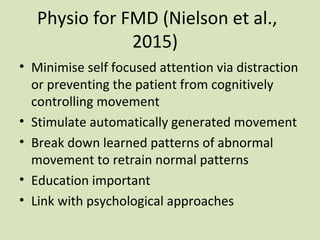
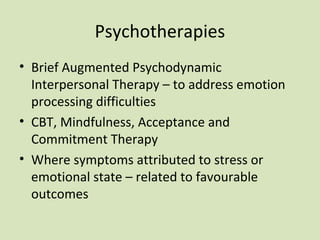
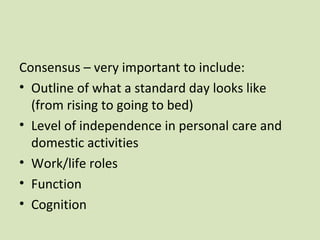
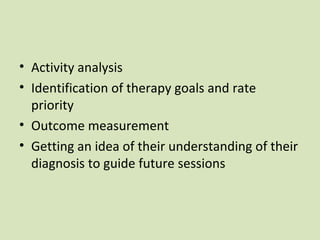
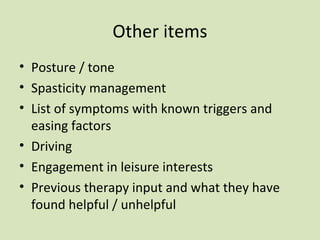
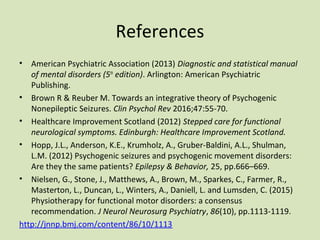
This document discusses functional neurological symptoms in multiple sclerosis. It defines functional neurological disorder and lists common signs and symptoms. Research shows that approximately 10% of neurology patients have a functional disorder. While initially thought to be purely psychiatric, functional disorders are now understood to involve both neurological and psychological factors. The cerebellum and limbic system may play a role in converting emotions into physical sensations. Occupational therapy aims to comprehensively assess patients' functioning and identify treatment goals. Physiotherapy focuses on minimizing attention to symptoms and retraining normal movement patterns. Psychotherapies like CBT can help address emotional processing difficulties. Functional symptoms appear to exist on a continuum and may be more common in MS patients than previously recognized.