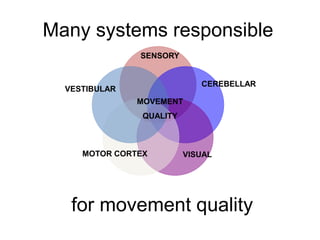
This document provides information on managing ataxia in multiple sclerosis (MS) through a multidisciplinary rehabilitation approach. It discusses the importance of managing ataxia to minimize social isolation and maximize quality of life. Assessment involves evaluating multiple body systems that can contribute to ataxia in MS. Interventions discussed include exercises to challenge balance, activities to improve coordination, strategies to compensate for impairments, and considerations for mobility aids, posture, eating, and cooling techniques. Evidence is presented supporting long-term rehabilitation to maximize potential and slow deterioration.