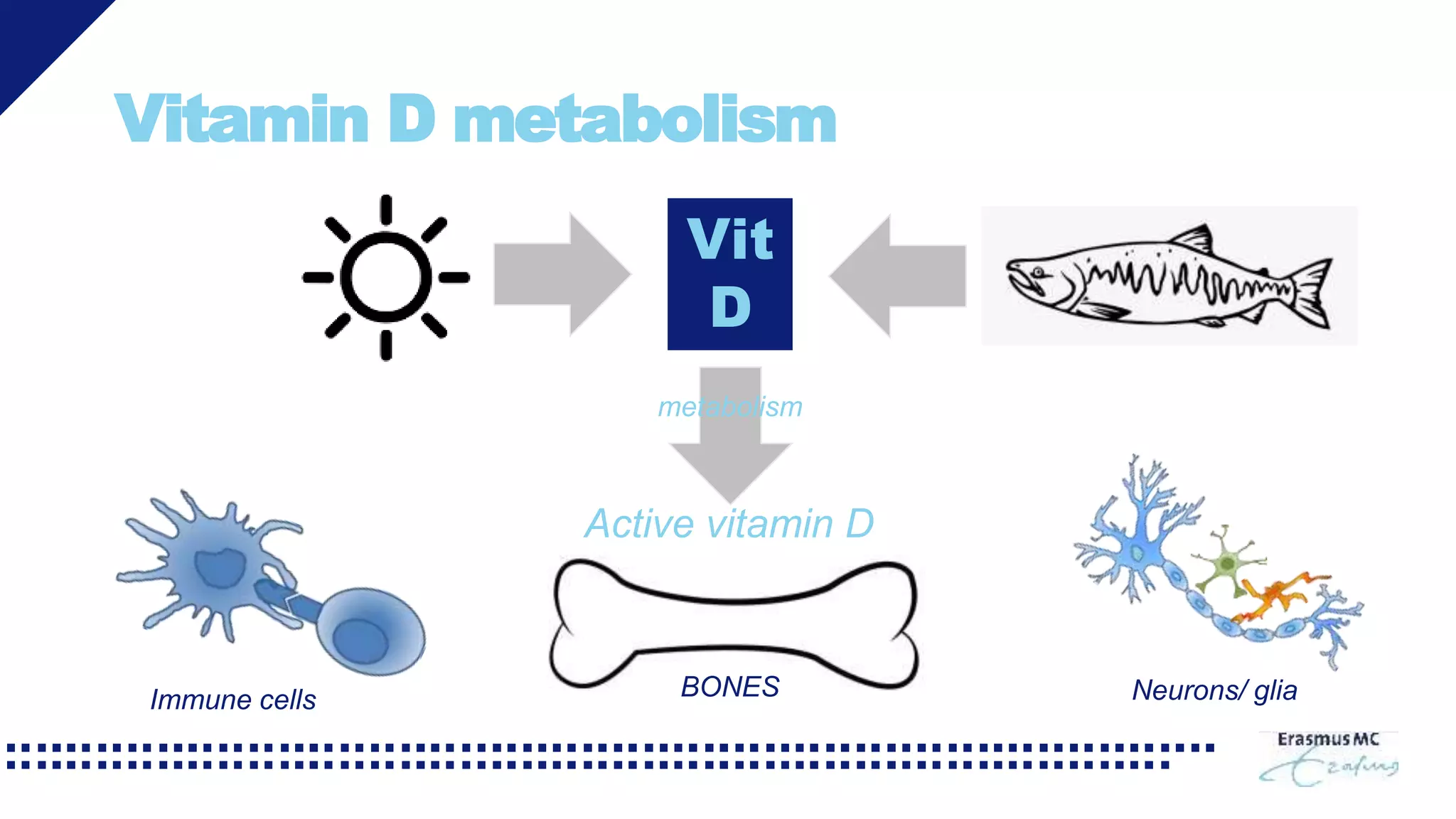
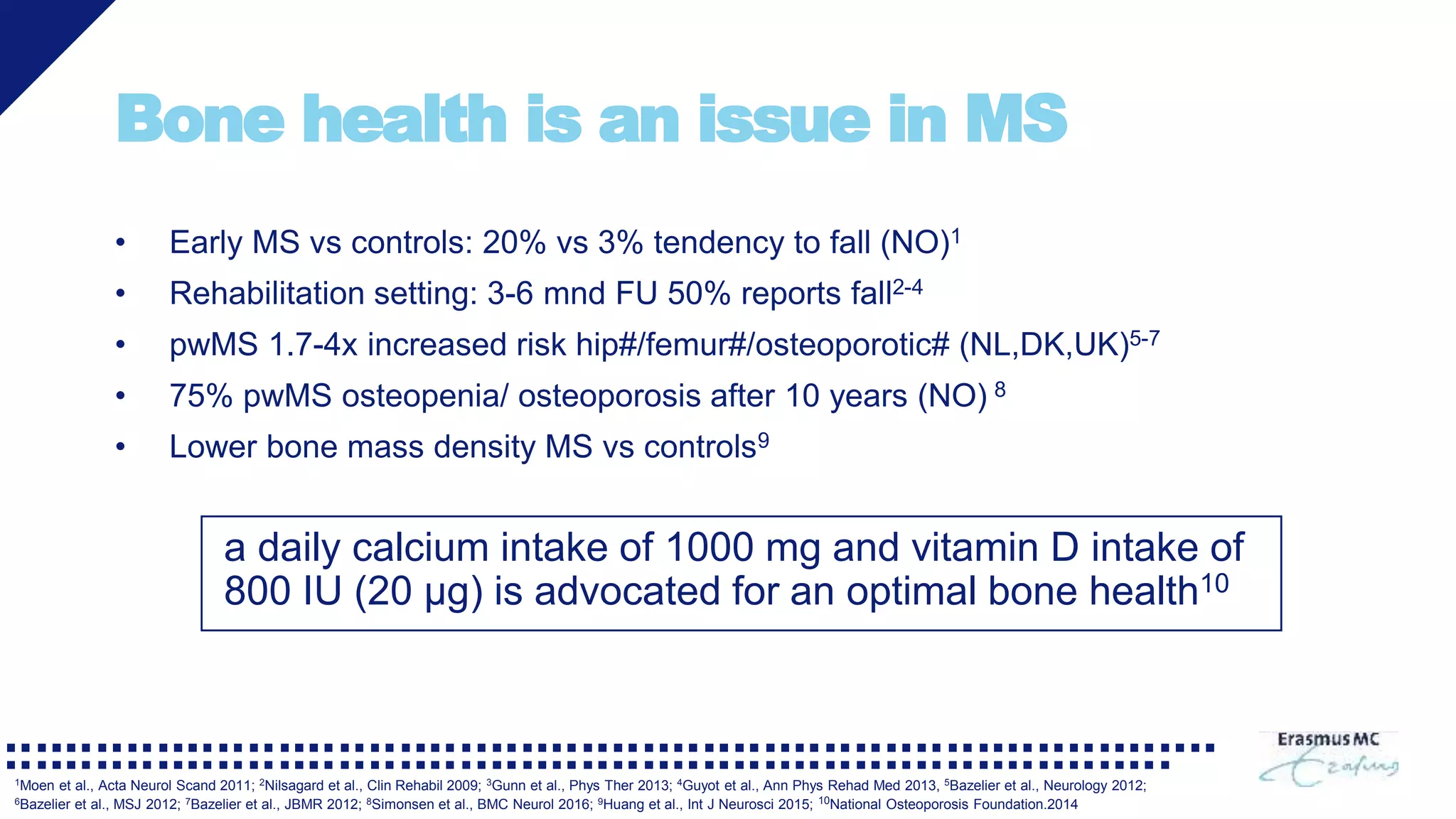
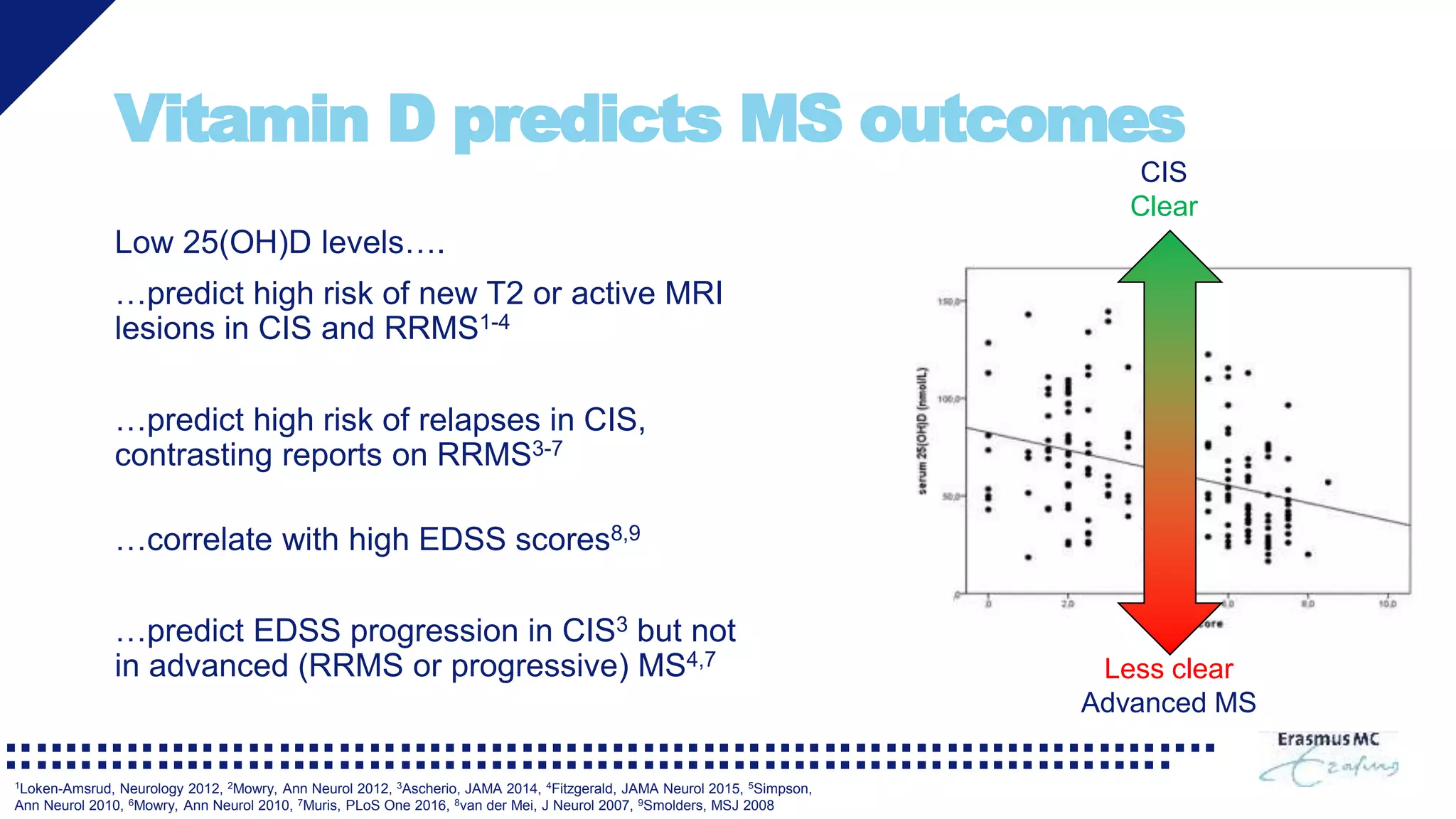
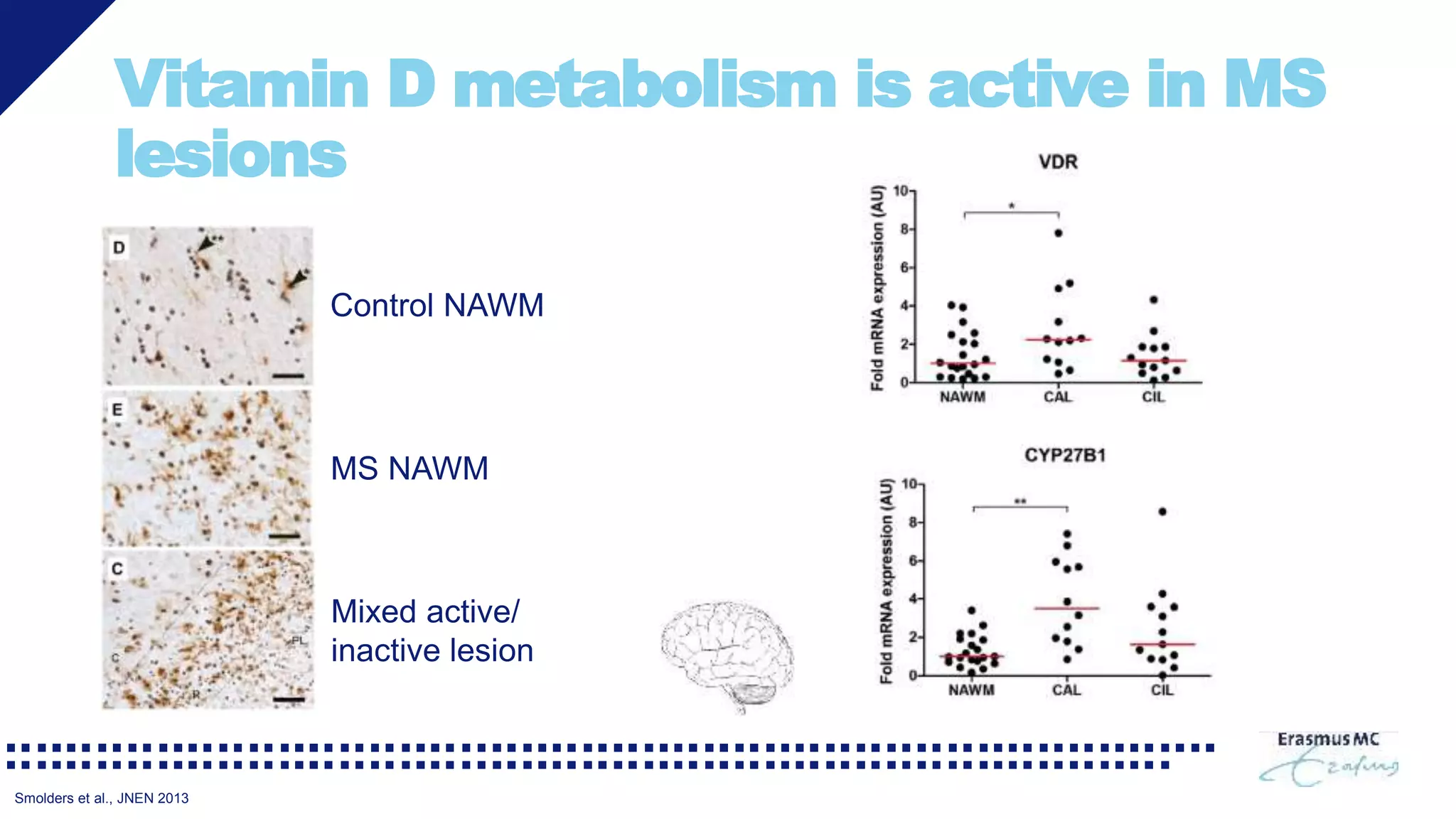
Vitamin D may have benefits for people with multiple sclerosis (MS). Low vitamin D levels are common in MS and are associated with worse bone health and increased disease activity. Supplementation to raise vitamin D levels has been shown to improve bone mineral density in MS. Some clinical trials also found signals that vitamin D supplementation may reduce MRI lesions and relapse rates. However, the evidence is mixed and high-dose supplementation over long periods may carry risks. Experts recommend MS patients aim to maintain vitamin D levels between 50-100 nM through supplementation as needed. More research is still needed to fully understand the role and optimal dosing of vitamin D in MS.