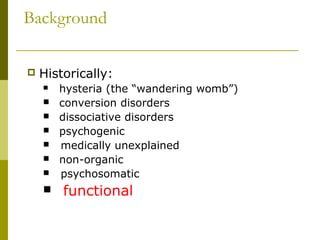
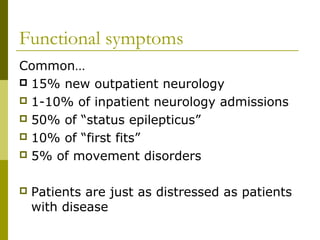
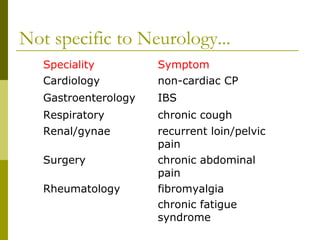
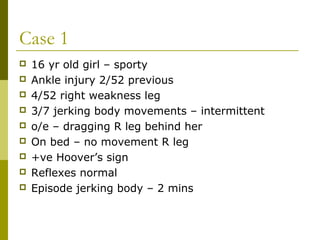
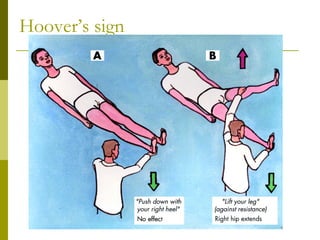
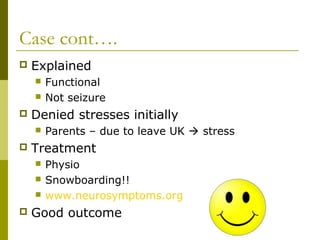
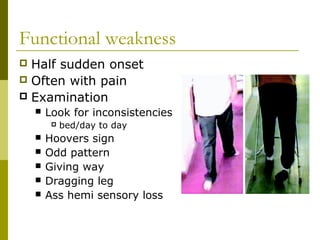
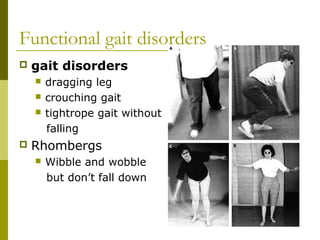
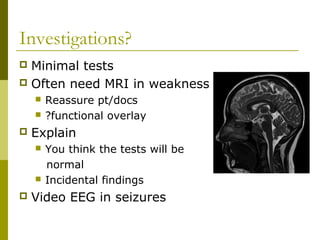
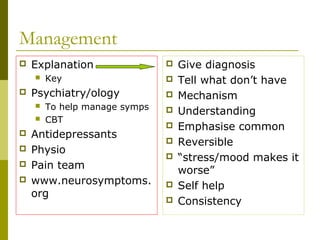
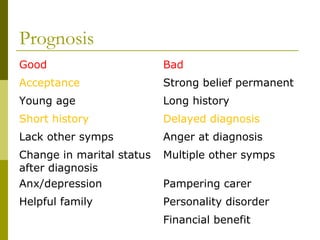
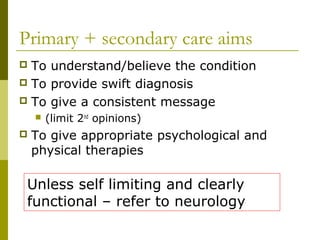
Functional neurology refers to neurological symptoms that are considered "functional" rather than due to identifiable organic disease. Two case studies are presented: a 16-year old girl with functional weakness and jerking movements, and a 34-year old woman with a sudden onset tremor. Investigations for functional disorders are typically minimal, while management involves explanation, psychiatry/psychology support like CBT, antidepressants, physiotherapy, and self-help resources. Prognosis is generally good, especially with early acceptance, short history, lack of other symptoms, and a supportive environment. The aims are to provide a swift diagnosis, consistent messaging to limit second opinions, and appropriate physical and psychological therapies.