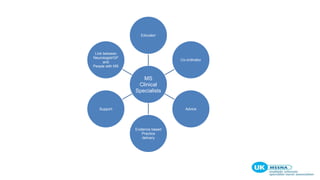
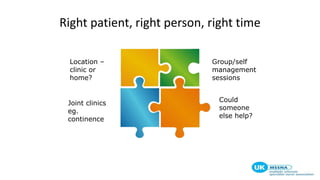
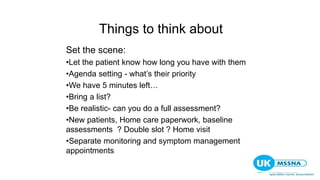
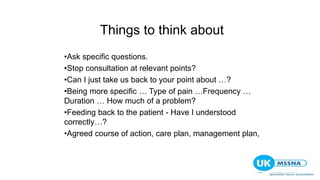
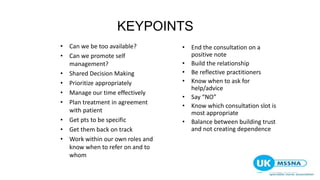
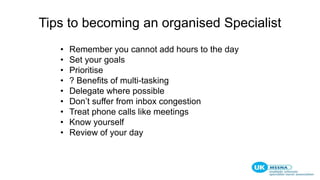
This document summarizes a skills development workshop for MS nurses that aimed to help them manage challenges in their roles. The workshop covered: identifying challenges MS nurses face in consultations and managing time/admin duties; tips for effective consultations including communication skills, managing patient dependence, and ending consultations; ways to manage time including organization, delegation, and auditing services; and sources of ongoing learning, development, and support for MS nurses.