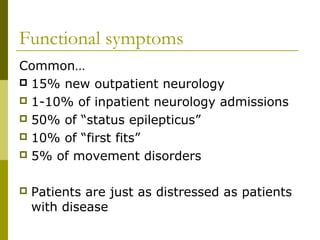
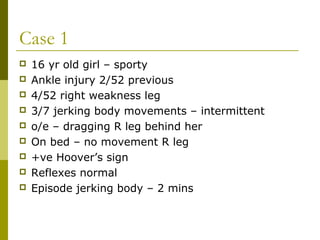
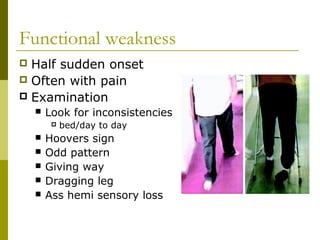
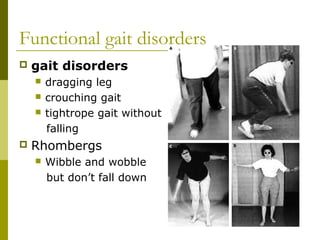
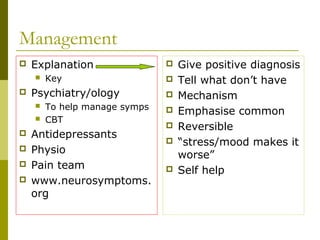
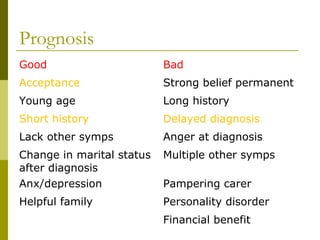
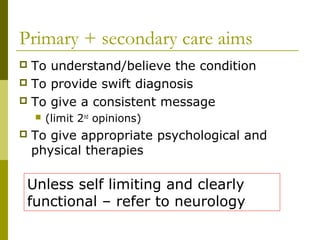
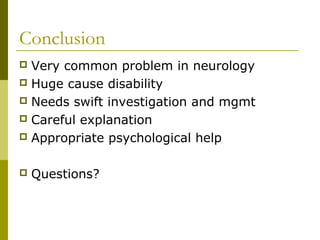
Functional neurology refers to neurological symptoms that are considered "functional" rather than caused by identifiable disease. Two case studies are presented: a 16-year old girl with right leg weakness and jerking movements found to have a functional disorder, and a 34-year old woman with a sudden onset right hand tremor. Common functional symptoms include weakness, gait disorders, tremors, and non-epileptic seizures. Investigations often show normal results, while management involves explanation, psychiatry or psychology referral, physiotherapy, and emphasizing the symptoms are common, reversible, and made worse by stress.